目的 探讨红细胞分布宽度(RDW)对急性脑梗死患者近期预后的预测价值。方法 回顾性纳入2016-01—2017-03于郑州大学第五附属医院神经内科住院的急性脑梗死患者169例,根据改良Rankin 量表(modified Rankin Scale,mRS)评分标准,分为预后良好组(104例)和预后不良组(65例)。比较2组入院时的年龄、性别、既往病史、美国国立卫生研究院卒中量表(NIHSS)评分、RDW等资料。采用多因素Logistic回归分析急性脑梗死预后不良的危险因素,采用受试者工作特征(ROC)
红细胞分布宽度对急性脑梗死患者近期预后的预测价值
柯俊吉 王建平△
郑州大学第五附属医院神经内科,河南 郑州 450052
基金项目:国家自然科学基金项目(81571137)
△通信作者:王建平(1956-),男,主任医师,神经病学博士,博士生导师。研究方向:脑血管病、癫痫、神经变性病、中枢神经系统感染、脱髓鞘疾病、周围神经病、脊髓疾病及神经遗传病等神经科疑难疾病的诊治。Email:wjpwfy666@126.com
【摘要】 目的 探讨红细胞分布宽度(RDW)对急性脑梗死患者近期预后的预测价值。方法 回顾性纳入2016-01—2017-03于郑州大学第五附属医院神经内科住院的急性脑梗死患者169例,根据改良Rankin 量表(modified Rankin Scale,mRS)评分标准,分为预后良好组(104例)和预后不良组(65例)。比较2组入院时的年龄、性别、既往病史、美国国立卫生研究院卒中量表(NIHSS)评分、RDW等资料。采用多因素Logistic回归分析急性脑梗死预后不良的危险因素,采用受试者工作特征(ROC)曲线评价入院RDW水平对急性脑梗死患者预后不良的预测价值。结果 (1)与预后良好组相比,预后不良组入院时NIHSS评分、糖尿病占比率、高脂血症占比率、入院RDW水平均较高,差异均有统计学意义[6(4,9)分 vs 3(2,6)分;44.6%(29/65)vs 28.8%(30/104);43.1%(28/65)vs 26.0%(27/104);14.2%(13.5%,15.6%)vs 13.5%(12.7%,14.7%),P<0.05],其余指标组间比较差异均无统计学意义(P>0.05)。(2)多因素Logistic回归分析显示,入院NIHSS评分(OR值1.790,95% CI 1.388~2.309,P<0.001)及入院时RDW水平(OR值1.629,95% CI 1.052~2.521,P<0.05)是脑梗死预后不良的独立危险因素。(3)ROC曲线显示,入院RDW水平预测急性脑梗死患者近期预后不良的界值13.65%,敏感度70.8%,特异度60.6%。结论 入院时RDW水平升高对评估急性脑梗死患者近期预后不良具有一定的参考价值。
【关键词】 急性脑梗死;红细胞分布宽度;预后;Logistic回归分析;危险因素
【中图分类号】 R743.33 【文献标识码】 A 【文章编号】 1673-5110(2018)03-0253-05 DOI:10.12083/SYSJ.2018.03.065
Red blood cell distribution width for the predictive analysis of the prognosis in patients with acute cerebral infarction
KE Junji,WANG Jianping
Department of Neurology,the Fifth Affiliated Hospital of Zhengzhou University,Zhengzhou 450052,China
【Abstract】 Objective To investigate the predictive value of red cell distribution width (RDW)for the short-term prognosis of acute cerebral infarction patients.Methods A total of 169 cases of acute cerebral infarction diagnosed at admission in the Department of Neurology,the Fifth Affiliated Hospital of Zhengzhou University from January 2016 to March 2017 were enrolled retrospectively.They were divided into ether a good prognosis group (n=104) or a poor prognosis group (n=65) according to the scoring criteria of the modified Rankin scale (mRS).The age,gender,past medical history,National Institutes of Health stroke scale (NIHSS) score and RDW were collected on admission.Multivariate logistic regression analysis was used to analyze the risk factors of poor prognosis of acute cerebral infarction.Receiver operating characteristic curve (ROC) was used to evaluate the predictive value of the RDW level for patients with acute cerebral infarction on admission.Results Compared with the good prognosis group,NIHSS score on admission,incidence of Diabetic history,incidence of hyperlipidemia history and RDW levels on admission in the poor prognosis group were significantly higher[6(4,9)vs.3(2,6);44.6%(29/65)vs.28.8%(30/104);43.1%(28/65)vs.26.0%(27/104);14.2%(13.5%,15.6%)vs.13.5%(12.7%,14.7%);all P<0.05].There were no significant differences in other indexes between the groups(all P>0.05).Multivariate logistic regression analysis showed that the NIHSS score on admission (OR 1.790,95% CI were 1.388-2.309,P<0.001)and RDW level on admission(OR 1.629,95% CI were 1.052-2.521,P<0.05),were independent risk factors for poor prognosis.ROC curve analysis showed that the diagnostic cut-off value of the RDW level on admission for the poor prognosis in patients with acute ischemic stroke was 13.65%.Its sensitivity was 70.8% and specificity was 60.6%.Conclusion Increased RDW at admission had certain reference function on the recent poor prognosis in patients with acute cerebral infarction.
【Key words】 Acute cerebral infarction;Red cell distribution width;Prognosis;Logistic models;Risk factors
脑梗死是脑卒中的一个重要类型,具有高发病率、高致残率以及高病死率的特点[1]。红细胞分布宽度(red blood cell distribution width,RDW)是反映外周血红细胞体积大小的特异性指标,主要应用于贫血的诊断和鉴别诊断[2]。近年来,RDW被证实与心力衰竭[3]、心肌梗死[4]、心房颤动[5]、外周动脉疾病[6]及肾脏损害[7]患者的预后都有相关性。本研究拟探讨入院时RDW水平对急性脑梗死患者近期预后的预测作用。
1 对象与方法
1.1 对象 回顾性纳入2016-01—2017-03于郑州大学第五附属医院神经内科住院的急性脑梗死患者169例,男112例,女57例;年龄46~86(66.92±7.365)岁。按照TOAST分型标准[8]进行卒中病因学分型,大动脉粥样硬化型脑梗死76例,小血管闭塞型脑梗死63例,心源型卒中3例,其他原因型脑梗死4例,不明原因型脑梗死23例。根据改良Rankin 量表(mRS)评分标准[9],分为预后良好组(104例)和预后不良组(65例)。预后良好组男70例,女34 例;预后不良组男42 例,女23例。纳入标准: (1)符合缺血性脑卒中的诊断标准[10],并经头部CT或MRI证实。(2)发病≤72 h;(3)入院时出现局灶性神经功能缺损症状和体征。排除标准:(1)进行溶栓治疗;(2)复发型脑梗死;(3)各种贫血症、严重肝肾功能不全以及近期用铁、叶酸、维生素B12补充治疗;(4)入院前1个月内有明确感染史;(5)合并恶性肿瘤;(6)伴有血液系统疾病、免疫系统疾病及结缔组织病;(7)妊娠患者;(8)入院前3个月内有外伤、手术及输血史。
1.2 资料收集 收集患者入院时年龄、性别、既往病史、烟酒史、家族史、入院时血压、发病到入院时间、入院15 min内NIHSS评分[11]等一般资料,以及患者入院24 h 内血常规、空腹血糖等实验室检查数据。根据改良Rankin量表评分情况分为预后良好组(mRS≤2分)和预后不良组(mRS>2分)。
1.3 统计学处理 采用SPSS 21.0软件包进行数据处理。正态分布的计量资料以均数±标准差(x±s)表示,组间比较采用独立样本t检验;偏态分布的计量资料采用中位数及四分位数[M(P25,P75)]表示,组间比较采用Mann-Whitney U检验;计数资料采用频数(%)表示,组间比较采用χ2检验或Fisher检验。采用多因素Logistic回归方程,分析急性脑梗死患者预后不良的危险因素,计算优势比(odds ratio,OR)和95%可信区间(confidence interval,CI)。采用ROC曲线评价入院时RDW对急性脑梗死患者预后不良的敏感度及特异度,并计算Youden指数,确定诊断最佳界值。P<0.05为差异有统计学意义。
2 结果
2.1 2组临床资料比较 与预后良好组比较,预后不良组患者入院时NIHSS评分、糖尿病占比、高脂血症占比、入院RDW水平均较高,差异均有统计学意义(P<0.05),其余指标的组间比较差异无统计学意义(P>0.05)。见表1。
表1 2组临床资料比较
| 资料 |
预后良好组(n=104) |
预后不良组(n=65) |
t/Z/χ2值 |
P值 |
| 年龄/岁(x±s) |
66.67±7.386 |
67.32±7.327 |
-0.557a |
0.578 |
| 男性[n(%)] |
70(67.3) |
42(64.6) |
0.130b |
0.74 |
| 高血压[n(%)] |
72(69.2) |
51(78.5) |
1.720b |
0.217 |
| 糖尿病[n(%)] |
30(28.8) |
29(44.6) |
4.377b |
0.047 |
| 冠心病[n(%)] |
34(32.7) |
24(36.9) |
0.318b |
0.619 |
| 高脂血症[n(%)] |
27(26.0) |
28(43.1) |
5.338b |
0.028 |
| 吸烟史[n(%)] |
29(27.9) |
20(30.8) |
0.162b |
0.729 |
| 饮酒史[n(%)] |
21(20.2) |
16(24.6) |
0.567b |
0.458 |
| TOAST分型[n(%)] LAA |
47(45.2) |
29(44.6) |
2.157b |
0.749 |
| SAA |
37(35.6) |
26(40.0) |
|
|
| CE |
1(1.0) |
2(3.1) |
|
|
| SOE |
3(2.9) |
1(1.5) |
|
|
| SUE |
16(15.4) |
7(10.8) |
|
|
| 血压[mmHg,M(P25,P75)] 收缩压 |
150(134,168) |
154(139,170) |
-1.631c |
0.103 |
| 舒张压 |
88(80,95) |
90(80,98) |
-1.157c |
0.248 |
| 发病到入院时间[h,M(P25,P75)] |
10(4.25,17) |
7(3,16) |
-1.592c |
0.112 |
| 入院NIHSS评分[M(P25,P75)] |
3(2,6) |
6(4,9) |
-4.699c |
<0.001 |
| 红细胞分布宽度[%,M(P25,P75)] |
13.5(12.7,14.7) |
14.2(13.5,15.6) |
-3.645c |
<0.001 |
| 空腹血糖[mmol/L,M(P25,P75)] |
5.4(5.0,7.275) |
6.1(5.3,7.35) |
-1.861c |
0.063 |
注:TOAST为国际急性卒中Org 10172 治疗试验;LAA 为大动脉粥样硬化型;SAA为小动脉闭塞型;CE为心源型;SOE为其他原因型;SUE为不明原因型;a为t值;b为χ2值;c为Z值
2.2 急性脑梗死预后不良的危险因素分析 以表1中P<0.05的变量为自变量,急性脑梗死患者预后不良为因变量,行多因素Logistic回归分析显示,入院NIHSS评分及入院RDW水平增高是急性脑梗死患者近期预后不良的独立危险因素(P<0.05)。见表2。
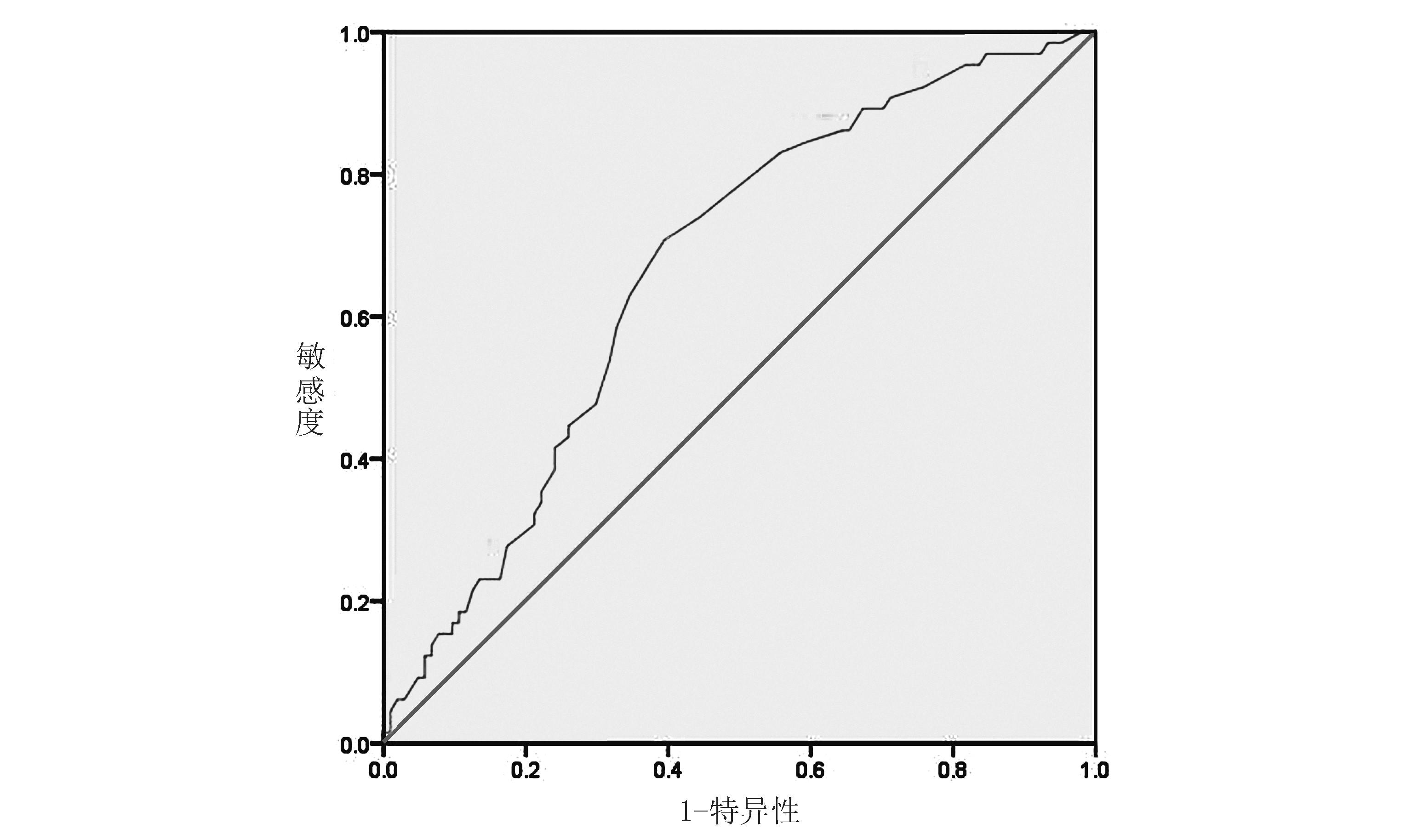
2.3 入院时RDW水平对急性脑梗死患者预后的预测分析 ROC曲线下面积为0.667(0.585~0.749),当入院RDW水平预测界值为13.65时,获得最大Youden指数0.313,敏感度70.8%,特异度60.6%。见图 1。
表2 急性脑梗死患者预后不良的危险因素分析
| 影响因素 |
OR值 |
95% CI |
P值 |
| 入院NISS评分 |
1.79 |
1.388~2.309 |
<0.001 |
| 入院RDW |
1.629 |
1.052~2.521 |
0.029 |
| 糖尿病史 |
0.087 |
0.006~1.274 |
0.075 |
| 高脂血症 |
0.158 |
0.012~1.995 |
0.154 |
图1 入院时RDW预测急性脑梗死患者预后的受试者工作特征曲线
3 讨论
高RDW水平与脑梗死患者预后不良的病理生理机制尚不明确,考虑与炎症、氧化应激、高凝状态、肾素-血管紧张素-醛固酮系统激活有关。炎症反应、氧化应激是动脉粥样硬化发展的主要因素[12-13],是缺血性脑卒中重要的病理发展机制[14-15]。RDW水平的增高与颈动脉粥样硬化斑块的不稳定性密切相关[16-18],可能反映一种潜在的炎性反应状态。LIPPI等[19]描述了RDW和炎症标记物之间的关系,如超敏C反应蛋白(hsCRP)和红细胞沉降率(ESR)等。炎症反应会削弱铁代谢、减少促红细胞生成素的产生、降低骨髓红系干细胞对促红细胞生成素刺激的敏感性、促进红细胞凋亡,使不成熟的红细胞进入循环,导致无效增生及异质性增加从而使RDW升高[20-23]。除炎性反应,氧化应激也可能在红细胞异质性方面起到重要作用。氧化应激会引起红细胞膜破坏,导致红细胞脆性增高,从而降低红细胞成熟率并缩短红细胞寿命,导致RDW增高[24]。另外,RDW升高伴随血红蛋白携氧量减少、红细胞变形能力降低,促进红细胞凝集,从而导致血流速度减慢,引起微循环的血流灌注不足甚至导致血管闭塞[25-26]。红细胞是血栓的组成成分,红细胞大小不均可能会增加红细胞的血栓形成作用[27]。肾素血管紧张素系统的激活增加可能是另一种对RDW和脑卒中之间联系的解释。肾素血管紧张素系统的激活促进了一个血栓形成的状态,增加缺血性脑卒中和脑出血的风险[28-29]。同时,激活的肾素血管紧张素系统通过对红细胞生成素水平的调节和对红系祖细胞的直接刺激两种途径导致红细胞增多和RDW升高[30-31]。
本研究初步探讨入院时RDW水平与急性脑梗死患者近期预后的相关性,其最佳预测值为13.65%,即入院时RDW水平>13.65时提示急性脑梗死患者预后不良的风险较大,与国内外既往研究一致[32-34]。
RDW是一个便捷、价廉的临床预测指标,入院时RDW水平可反映急性脑梗死患者机体内慢性炎症、氧化应激、高凝状态、神经体液激活的程度。对入院RDW水平偏高的急性脑梗死患者早期采取积极干预措施,可能会改善患者预后。然而,本研究为单中心研究,样本量较少,仅对入院时RDW水平进行探讨,缺乏动态观察,尚需进一步大样本多中心研究分析RDW水平与急性脑梗死患者预后的相关性。
4 参考文献
[1] 陈洪苹,钟镝,李国忠.单中心脑梗死住院患者病死率及死因分析[J].中国脑血管病杂志,2015,12(2):62-66.
[2] SALVAGNO G L,SANCHIS-GOMAR F,PI-CANZA A,et al.Red blood cell distribution width: A simple parameter with multiple clinical applications[J].Crit Rev Clin Lab Sci,2015,52(2):86-105.
[3] KAYA A,ISIK T,KAYA Y,et al.Relationship Between Red Cell Distribution Width and Stroke in Patients With Stable Chronic Heart Failure:A Propensity Score Matching Analysis[J].Clin Appl Thromb Hemost,2015,21(2):160-165.
[4] HU G X,ZHANG J,TIAN Y G,et al.Diagnostic value of joint detection of homocysteine and RDW CV on acute myocardial infarction[J].Eur Rev Med Pharmacol Sci,2016,20(19):4 124-4 128.
[5] SARIKAYA S,SAHIN S,AKYOL L,et al.Is there any relationship between RDW levels and atrial fibrillation in hypertensive patients[J].Afr Health Sci,2014,14:267-272.
[6] ZALAWADIYA S K,VEERANNA V,PANAICH S S,et al.Red cell distribution width and risk of peripheral artery disease: analysis of National Health and Nutrition Examination Survey 1999-2004[J].Vasc Med,2012,17(3):155-163.
[7] ZHANG M,ZHANG Y,LI C,et al.Association between red blood cell distribution and renal function in patients with untreated type 2 diabetes mellitus[J].Ren Fail,2015,37(4):659-663.
[8] ADAMS H P,Jr,BENDIXEN B H,KAPPELLE L J,et al.Classification of subtype of acute ischemic stroke.Definitions for use in a multicenter clinical trial.TOAST.Trial of Org 10172 in Acute Stroke Treatment[J].Stroke,1993,24(1):35-41.
[9] VAN SWIETEN J C,KOUDSTAAL P J,VISSER M C,et al.Interobserver agreement for the assessment of handicap in stroke patients[J].Stroke,1988,19(5):604-607.
[10] 中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组.中国急性缺血性脑卒中诊治指南2014[J].中华神经科杂志,2015,48(4):246-257.
[11] WILLIAMS L S,YILMAZ E Y,LOPEZ-YUNEZ A M.Retrospective assessment of initial stroke severity with the NIH Stroke Scale[J].Stroke,2000,31(4):858-862.
[12] 陈瑗,周玫.氧化应激-炎症在动脉粥样硬化发生发展中作用研究的新进展[J].中国动脉硬化杂志,2008,16(10):757-762.
[13] PACKARD R R,LIBBY P.Inflammation in atherosclerosis:from vascular biology to biomarker discovery and risk prediction[J].Clin Chem,2008,54(1):24-38.
[14] LINDSBERG P J,GRAU A J.Inflammation and infections as risk factor for ischemic stroke[J].Stroke,2003,34:2 518-2 532.
[15] CHEN C Y,CHEN C L,YU C C,et al.Association of inflammation and oxidative stress with obstructive sleep apnea in ischemic stroke patients[J].Sleep Med,2015,16(1):113-118.
[16] 宋芷珩,范凌霄.红细胞分布宽度和脑梗死患者颈动脉粥样硬化斑块稳定性的关系[J].中风与神经疾病杂志,2015,32(8):708-711.
[17] 王鹏,吕卫华,刘和锦,等.老年脑梗死患者颈动脉粥样硬化斑块稳定性与红细胞分布宽度的关系[J].中华老年心脑血管病杂志,2013,5(5):488-491.
[18] BONAQUE J C,PASCUAL FIGAL D A,MANZANO FERNDNDEZ S,et al.Red blood cell distribution width adds prognostic value for out patients with chronic heart failure[J].Rev Esp Cardiol(Engl Ed),2012,65(7):606-612.
[19] LIPPI G,TARGHER G,MONTAGNANA M,et al.Relation between red blood cell distribution width and inflammatory biomarkers in a large cohort of unselected outpatients[J].Arch Pathol Lab Med,2009,133(4):628-632.
[20] EMANS M E,VAN DER PUTTEN K,VAN ROOIJEN K L,et al.Determinants of Red Cell Distribution Width(RDW)in cardiorenal patients:RDW is not related to erythropoietin resistance[J].J Card Fail,2011,17(8):626-633.
[21] KIM C H,PARK J T,KIM E J,et al.An increase in red blood cell distribution width from baseline predicts mortality in patient with severe sepsis or septic shock[J].Cirt Care,2013,17(6):R282.
[22] ODBAYAR T O,BADAMHAND D,KIMURA T,et al.Comparative studies of some phenolic compounds (quercetin,rutin,and ferulic acid)affecting hepatic fatty acid synthesis in mice[J].J Agric Food Chem,2006,54(21):8 261-8 265.
[23] EPHREM G.Red blood cell distribution width should indeed be assessed with other inflammatory markers in daily clinical practice [J].Cardiology,2013,124(1):61.
[24] FRIEDMAN J S,LOPEZ M F,FLEMING M D,et al.SOD2-deficiency anemia: protein oxidation and altered protein expression reveal targets of damage,stress response,and antioxidant responsiveness[J].Blood,2004,104(8):2 565-2 573.
[25] REZENDE S M,LIJFERING W M,ROSENDAAL F R,et al.Hematologic variables and venous thrombo-sis:red cell distribution width and blood monocyte count are associated with an increased risk[J].Haematologica,2014,99(1):194-200.
[26] YEDGAR S,KOSHKARYEV A,BARSHTEIN G.The red blood cell in vascular occlusion[J].Patho-physiol Haemost Thromb,2002,32(5/6):263-268.
[27] ZLLER B,MELANDER O,SVENSSON P,et al.Red cell distribution width and risk for venous thromboembolism:a population-based cohort study[J].Thromb Res,2014,133(3):334-339.
[28] PARK H K,KIM M C,KIM S M,et al.Assessment of two missense polymorphisms(rs4762 and rs699) of the angiotensinogen gene and stroke[J].Exp Ther Med,2013,5:343-349.
[29] WANG Y L,HUA Q,BAI C R,et al.Relationship between red cell distribution width and short-term outcomes in acute coronary syndrome in a Chinese population[J].Intern Med,2011,50(24):2 941-2 945.
[30] PARK T S,ZAMBIDIS E T.A role for the renin-angiotensin system in hematopoiesis[J].Haematologica,2009,94:745-747.
[31] KATO H,ISHIDA J,IMAGAWA S,et al.Enhanced erythropoiesis mediated by activation of the renin-angiotensin system via angiotensin Ⅱ type 1a receptor[J].FASEB J,2005,19:2 023-2 025.
[32] KIM J,KIM Y D,SONG T J,et al.Red blood cell distribution width is associated with poor clinical outcome in acute cerebral infarction[J].Thromb Haemost,2012,108(2):349-356.
[33] 丁勇,王飞,胡善友.红细胞分布宽度与脑梗死患者近期预后的相关性[J].中华老年多器官疾病杂志,2013,12(11):810-813.
[34] 王飞,俞青,吴晓,等.老年脑梗死严重偏瘫患者的红细胞分布宽度与预后的相关性[J].中国脑血管病杂志,2015,12(6):287-291.
(收稿2017-09-11 修回2017-12-15)
本文编辑:夏保军
本文引用信息:柯俊吉,王建平.红细胞分布宽度对急性脑梗死患者近期预后的预测价值[J].中国实用神经疾病杂志,2018,21(3):253-257.