目的 探讨巨大型颅内动脉瘤的临床特点和显微手术治疗的策略。方法 回顾分析大连大学附属中山医院2006-01—2017-06收治的36例巨大动脉瘤患者,均采取显微外科手术治疗。结果 36例巨大型颅内动脉瘤手术均成功,无死亡,出院时优良31例,轻残5例。结论 对于巨大型颅内动脉瘤术前充分准备,采取正确的手术方法和技巧,可以获得良好的手术效果。
巨大型颅内动脉瘤显微外科手术临床分析
李彦钊 孙丕通 邓东风 孙 晶 郎明非 曲晓扬 张绪新△
大连大学附属中山医院神经外科,辽宁大连 116001
基金项目:国家自然科学基金(编号:21505013);辽宁省科学技术基金(编号:2015020660)
作者简介:李彦钊,Email:510133106@qq.com
△通信作者:张绪新,Email:13842623672@163.com
【摘要】 目的 探讨巨大型颅内动脉瘤的临床特点和显微手术治疗的策略。方法 回顾分析大连大学附属中山医院2006-01—2017-06收治的36例巨大动脉瘤患者,均采取显微外科手术治疗。结果 36例巨大型颅内动脉瘤手术均成功,无死亡,出院时优良31例,轻残5例。结论 对于巨大型颅内动脉瘤术前充分准备,采取正确的手术方法和技巧,可以获得良好的手术效果。
【关键词】 颅内动脉瘤;巨大动脉瘤;显微外科;开颅夹闭;手术技巧
【中图分类号】 R739.41 【文献标识码】 A 【文章编号】 1673-5110(2018)24-2681-05 DOI:10.12083/SYSJ.2018.24.560
Clinical analysis of microsurgical treatment of giant intracranial aneurysms
LI Yanzhao,SUN Pitong,DENG Dongfeng,SUN Jing,LANG Mingfei,QU Xiaoyang,ZHANG Xuxin
Affiliated Zhongshan Hospital of Dalian University,Dalian 116001,China
【Abstract】 Objective To explore the strategies and methods of microsurgical treatment of giant intracranial aneurysms malformations.Methods A retrospective analysis of 36 patients with giant aneurysms admitted to Zhongshan Hospital of Dalian University from January 2006 to June 2017 treated by microsurgery was made.Results The neurosurgical operation succeed.No patients died.Outcome was considered as good in 31 cases,fair in 5 cases.Conclusion With sufficient pre-operative examination,correct operatives and technique,the giant intracranial aneurysms can be treated effectively with good results.
【Keys words】 Intracranial aneurysm;Giant aneurysm;Microsurgery;Clipping;Surgical technique
巨大型颅内动脉瘤(giant intracranial aneurysm)是指瘤体最大直径>25 mm的动脉瘤,临床主要表现为出血、缺血及占位效应,发生率占颅内动脉瘤的3%~13.5%[1-2]。由于巨大动脉瘤体积大,占位效应明显,分离过程中极易破裂出血,手术难度大,致残、致死率高,KATZB等[3]报道对于巨大型动脉瘤,动脉瘤不全夹闭率和载瘤动脉狭窄率高达15%以上。本文回顾分析大连大学附属中山医院2006-01—2017-06收治的36例巨大动脉瘤患者,均成功行开颅手术夹闭、切除。
1 资料与方法
1.1 一般资料 本组36例巨大颅内动脉瘤患者,男17例,女19例;年龄22~76岁,平均43.6岁;首发症状:癫痫7例,脑出血3例,头痛3例,神经功能障碍2例。
1.2 临床表现 以自发性蛛网膜下腔出血为首发症状21例,动眼神经麻痹4例,癫痫2例,头痛3例,肢体偏瘫2例,视力下降4例,意识障碍1例。
1.3 影像学资料 术前影像学资料包括头部CT、MRI、CTA以及DSA,所有患者术前行CTA和(或)DSA检查后进行动脉瘤测量,直径均>25 mm。其中合并血管畸形2例,普通动脉瘤8例;巨大型动脉瘤位于颈内动脉海绵窦段6例,眼动脉段5例,后交通段11例,脉络膜前动脉段3例,大脑中动脉M1段3例,前交通段4例,基底动脉分叉处4例;动脉瘤最大者为右侧大脑中动脉M1段,颈宽约2 cm,大小约12.5 cm×7.0 cm×8.0 cm。
1.4 手术方法 36例患者均行开颅显微手术治疗,选择翼点入路或扩大翼点入路,采用直接瘤颈夹闭和塑形夹闭34例,行动脉瘤孤立血管重建术1例,包裹术1例。8例合并普通动脉瘤一期夹闭3例,二期夹闭5例。2例合并血管畸形二期手术切除1例,随诊观察1例。
2 结果
GOS评分情况:31例良好,4例轻残,无死亡。其中最大1例动脉瘤患者术前偏瘫、意识障碍,术后第2天清醒,1个月后行走自如。术后3个月复查CTA和(或)全脑血管造影证实颅内动脉瘤完全消失。
3 讨论
巨大型颅内动脉瘤是指最大外径>25 mm的颅内动脉瘤[4],具有显著占位效应,手术治疗不仅有血管性疾病的技巧,还有肿瘤性疾病的特点。由于巨大动脉瘤的显著占位效应,使手术空间狭小,分离、显露困难,加之动脉瘤颈宽、瘤体壁薄、易破裂出血、穿支血管及周围重要解剖结构的保护,使手术难度加大,致残率和病死率增高。手术成败的问题包括载瘤动脉近心端的控制、动脉瘤大小影响视野、动脉瘤颈宽泛、复杂的分支和穿支血管、腔内血栓形成、载瘤动脉壁粥样硬化及发育异常[5]。诸多研究报道动脉瘤破裂与其部位有关,前交通动脉及后交通动脉是动脉瘤破裂风险最高的部位[6-8]。此外,动脉瘤形状也被认为与动脉瘤的破裂相关[9]。MAHTA等[10]报道此类动脉瘤的病死率和致残率均为20%左右。SCOZZAFAVA等[11]报道有症状的巨大动脉瘤如不及时采取治疗措施,80%的患者5 a内死亡或完全丧失独立生活能力。研究报道,巨大动脉瘤的占位效应致肿块压迫现象2 a内达65%~100%,常由于脑缺血致神经功能障碍或由于SAH死亡[12]。VILLABLANCA等[13]研究显示相对于稳定的动脉瘤,不断生长的动脉瘤破裂风险增高达20倍。BRINJIKJI等[14]研究表明,直径>1 cm的增长颅内动脉瘤年破裂率显著高于直径<1 cm的动脉瘤,不规则动脉瘤的年破裂率显著高于囊性动脉瘤。因此,应采取积极的治疗措施。治疗方法有开颅手术夹闭及血管内弹簧圈栓塞。国际上两项大型临床试验BART及ISAT比较了两者的优劣,前者表明开颅手术夹闭动脉瘤有更高的夹闭率及更低的复发率,后者显示介入栓塞效果优于开颅夹闭术;但两种方法预后无明显区别[15-16]。术前血流动力学改变的评估非常重要,科学的手术方案是决定治疗效果的关键[17-18]。巨大动脉瘤治疗以开颅手术夹闭为主,不管对于破裂、未破裂动脉瘤,还是复杂动脉瘤等,手术夹闭被认为是能够对瘤体达到最好的循环上的解剖分离效果。因血管内治疗发展到今天,仍无法满意地闭塞巨大动脉瘤的瘤腔,且无法解决占位效应[19],但血管内治疗仍有不可或缺的辅助作用。对于宽颈动脉瘤,以往手术多采用支架辅助治疗,但动脉瘤复发率比开颅手术高。近年来,血流导向装置逐渐应用于临床,血流导向装置是一种密网支架,金属覆盖率达30%~50%,远高于传统支架[20-22]。本组择期手术患者术前常规行Matas试验,Matas试验可以增加患者对缺血的耐受能力,延长载瘤动脉临时阻断时间。球囊闭塞试验将同侧颈内动脉完全闭塞后观察患者的意识改变,从而判断患者对缺血的耐受能力,发现对有条件的患者术前行球囊闭塞试验是个很好的选择,可以避免Matas试验不确定性。但球囊闭塞试验有其局限性,不能了解血流代偿能力及代偿程度,不能在短时间内多次进行检查,有文献报道即使术前球囊闭塞试验阴性,仍有4%~15%的缺血事件发生[23]。
术前行全脑血管造影检查对术前评估意义重大,不仅可以了解动脉瘤内血流情况以及载瘤动脉、穿支动脉、瘤颈宽度等情况,DSA检查时还可以压迫病灶侧颈动脉,行对侧颈动脉造影术,了解前交通动脉及后交通动脉的侧支循环情况。侧支循环良好的病例,如果手术失败,即使做颈动脉闭塞也不会产生严重不良后果,这对于术者来说,无疑是一种安全保障,使术者无后顾之忧。
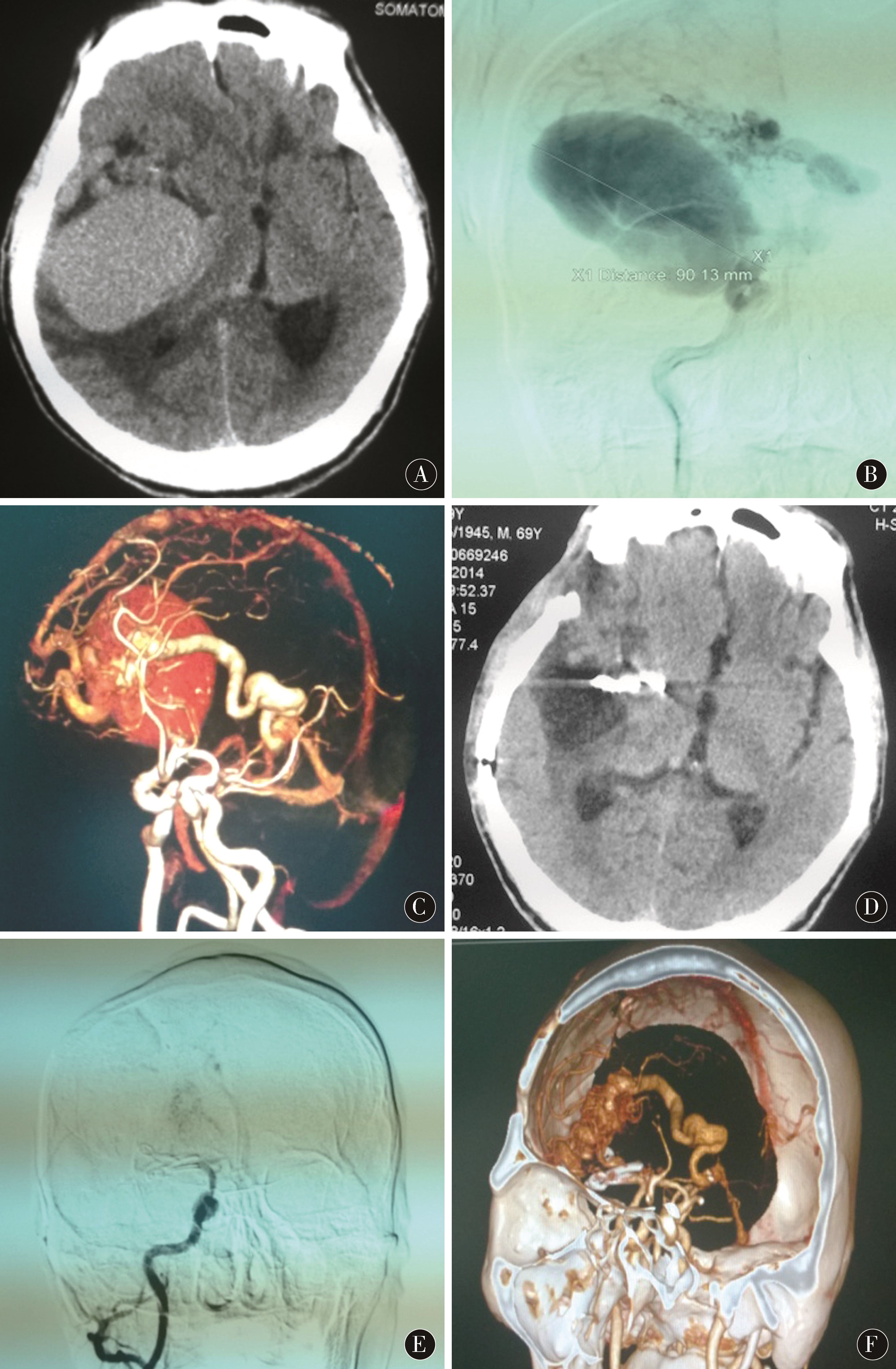
巨大动脉瘤体积大,位置深藏,常有重要穿支血管从其发出,瘤颈宽,瘤体形态不规则,常伴有血栓、钙化及粥样硬化改变,导致治疗难度大,预后差[24-25]。术前应根据头CT、MRI、CTA、DSA等检查制定周密的手术计划(图1A~C),包括手术入路选择、术中可能出现的风险。本组最大动脉瘤患者术前做详细讨论后制定了完善的术前准备,动脉瘤夹使用专门定制的超长夹,以确保手术万无一失。手术夹闭风险主要是围手术期动脉瘤破裂出血,在围手术期,尤其手术过程中自始至终都需要将防止动脉瘤破裂放在首位。全身麻醉、开颅过程中都会对颅内压产生影响,术中对破裂动脉瘤的紧急处理也很复杂,一旦处理不慎易导致手术失败或留下后遗症。即使手术夹闭成功,癫痫发生率也较高[26-28]。
图1 A:右侧大脑中动脉M1段巨大型动脉瘤术前CT平扫,占位效应明显;B~C:右侧大脑中动脉M1段巨大型动脉瘤术前DSA、 CTA示动脉瘤巨大合并血管畸形;D:巨大型动脉瘤术后CT平扫,占位效应解除;E~F:巨大型动脉瘤术后DSA、 CTA对比术前动脉瘤完全消失
Figure 1 A:The preoperative CT scan of the large aneurysm of the M1 segment of the right middle cerebral artery,the occupancy effect is obvious;B-C:Right cerebral artery M1 segment giant aneurysm preoperative DSA,CTA shows aneurysm huge vascular malformation;D:CT scan of giant aneurysm after operation,the effect of the occupancy is lifted;E-F:DSA,CTA,and preoperative aneurysm disappear completely after operation of giant aneurysm
手术疗效与病情分级、动脉瘤部位及术者技巧有密切关系。以本组最大的动脉瘤为例,为确保手术成功,先将颈内动脉颈段暴露待用,开颅剪开硬脑膜后,于脑表面可见部分动脉瘤瘤体分离侧裂,缓慢释放脑脊液,待脑组织塌陷完全后,牵开额叶及颞叶,暴露颈内动脉、右侧大脑中动脉M1段,向远心端分离至M1分叉处可见一支血管膨大形成动脉瘤,颈宽约2 cm,分离瘤颈后,先行阻断大脑中动脉近心端,以两枚特制动脉瘤夹夹闭动脉瘤,之后分离瘤体,剖开动脉瘤壁,见动脉瘤内血液分层,部分血栓形成,切除动脉瘤及瘤内血栓,术后复查相关血管检查,动脉瘤完全消失(图1D~F)。
有文献报道,动脉瘤的瘤囊巨大,瘤囊内血栓、钙化,并有重要分支血管发出无法塑形夹闭,可采用搭桥、动脉瘤近端夹闭或孤立的手术方法[29-32]。对薄壁无血栓动脉瘤直接穿刺瘤体抽吸,对血栓性动脉瘤可行瘤体切开取栓减压使瘤体塌陷,动脉瘤塑形后放置动脉瘤夹。术后给予预防血管痉挛是必不可少的治疗方法。夹闭过程必须确保血管主干及分支无堵塞,从血管内侧壁发出的所有穿支动脉没有被瘤夹叶片夹住。颅内大型及巨大型动脉瘤有两种类型,一种是血栓性动脉瘤,一种是非血栓性动脉瘤。血栓性动脉瘤发生率是非血栓性动脉瘤的1/3。一般认为是因动脉瘤巨大,动脉瘤瘤囊内出现“湍流”,致血流动力学改变,血液通过动脉瘤时速度减慢,逐渐形成。
本组巨大型颅内动脉瘤手术夹闭及切除成功,提示对于巨大型颅内动脉瘤患者,术前充分准备,采取正确的手术方法和技巧,可以获得良好的手术效果。
4 参考文献
[1] MOORE J M,CAPLAN L,HWANG P,et al.Dementia resulting from expansion of basilar artery aneurysm:two case reports and a review of lirerature[J].Acta Neurochir(Wien),2016,158(10):1 901-1 905.
[2] GRAZIANO F,GANAU M,IACOPINO D G,et al.Vertebro-basilar junction aneurysms:a single centre experience and meta-analysis of endovascular treatments[J].Neuroradiol J,2014,27(6):732-741.
[3] KATZ JM,GOLOGORSKY Y,TSIOURIS AJ,et al.Is routine intraoperative angiography in the surgical treatment of cerebral aneurysms justified.A consecutive series of 147 aneurysms[J].Neurosurgery,2006,58(4):719-727;discussion 719-727.
[4] SHARMA B S,GUPTA A,AHMAD F U,et al.Surgical management of giant intracranial aneurysms[J].Clin Neurol Neurosurg,2008,110(7):674-681.
[5] SUGHRUE M E,SALONER D,RAYZ V L,et al.Giant intracranial aneurysms:evolution of management in a contemporary surgical series[J].Neurosurgry,2011,69(6):1 261-1 270;discussion 1 270-1 271.
[6] JUVEAL S,POUSSA K,LEHTO H,et al.Natural History of unruptured intracranial aneurysms:a long-term follow-up study[J].Stroke,2013,44(9):2 414-2 421.
[7] WIEBERS D O,WHISNANT J P,HUSTON J,et al.Unruptured intracranial aneurysms:natural history,clinical outcome,and risk of surgical and endovascular treatment[J].Lancet,2003,362(9378):103-110.
[8] KANG H,JI W,QIAN Z,et al.Aneurysm Characte-ristics Associated with the Rupture Risk of Intracranial Aneurysms:A Self-Controlled Study[J].PLoS One,2015,10(11):e0142330.
[9] RAGHAVAN M L,MA B,HARBAUGH R E.Quantified aneurysm shape and rupture risk[J].J Neurosury,2005,102(2):355-362.
[10] MEHTA R I,SALAMON N,ZIPSER B D,et al.Giant intracranial aneurysm[J].Radiographics,2010,30(4):1 133-1 138.
[11] SCOZZAFAVA J,SUTHERLAND G A.Giant intracranial aneurysm[J].CMAJ,2011,183(9):E604.
[12] DARSAUT T E,DARSAUT N M.Clinical and angiographic outcome aftersurgical or endovascular therapy of verylarge and giant intracranial aneurysms[J].Neurosurgery,2011,68:903-915.
[13] VILLABLANCA J P,DUCKWILER G R,JAHAN R,et al.Natural history of asymptomatic unruptured cerebral aneurysms evaluated at CT angiography:growth and rupyure incidence and correlation with epidemiol-ogic risk factors[J].Radiology,2013,269(1):258-265.
[14] BRINJIKJI W,ZHU Y Q,LANZINO G,et al.Risk factors for growth of intracranial aneurysms:A systematic review and mata-analysis[J].AJNR Am J Neuroradiol,2016,37(4):615-620.
[15] MCDOUGALL C G,SPETZLER R F,ZABRAMSKI J M,et al.The Barrow Ruptured Aneurysm Trial[J].J Neurosury,2012,116(1):135-144.
[16] SPETZLER R F,MCDOUGALL C G,ALBUQUERQUE F C,et al.The Barrow Ruptured Aneurysm Trial:3-year results[J].J Neurosurg,2013,119(1):146-157.
[17] IMAI H,WATANABE K,MIYAGISHIMA T,et al.The outcome of a surgical protocol based on ischemia overprotection in large and giant aneurysms of the anterior cerebral circulation[J].Neurosurg Rew,2016,39(3):505-517.
[18] ZHU P X,LIU Y L,TIAN Y X,et al.Complex middle cerebral artery aneurysms:a new classification based on the angioarchitecture and surgical strategies[J].Acta Neurochirurgica,2013,155(8):1 481-1 491.
[19] HA S W,JANG S J.Clinical analysis of giant intracranial aneurysms with endovascular embolization[J].J Cerebrovasc Endovasc Neurosurg,2012,14(1):22-28.
[20] SIDDIQUI A H,KAN P,ABLA A A,et al.Complications after treatment With pipeline embolization for giant distal intracranial aneurysms with or whit or without coil embolization[J].Neurosurgery,2012,71(2):E509-E513.
[21] LYLYK P,MIRANDA C,CERATTO R,et al.Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device:the Buenos Aires experience[J].Neurosurgery,2009,64(4):632-642.
[22] SZIKORA I,BERENTEI Z,KULCSAR Z,et al.Treatment of intracranial aneurysms by functional reconstruction of the parent artery:the Budapest experience with the pipeline embolization device[J].AJNR Am J Neuroradiol,2010,31(6):1 139-1 147.
[23] GONZALEZ N R,DUCKWILER G,JAHAN R,et al.Challenges in the endovascular treatment of giant intracranial aneurysms[J].Neurosurgery,2006,59:113-124.
[24] HA S W,JING S J.Clinical analysis of giant intracra-nial ancurysms with endovascular embolization[J].J Cerebrovasc Endovasc Neurosurg,2012,14(1):22-28.
[25] NANDA A,SONIG A,BANERJEE A D,et al.Microsurgical management of basilar artery apex aneurysms:a signal surgeon’s experience from Louisiana State University,Shreveport[J].World Neurosurg,2014,82(1/2):118-129.
[26] MOLYNEUX A J,KERR R S,YU L M,et al.International subarachnoid aneurysm trial(ISAT) of neurosurgical clipping versus endovaseular coiling in 2143 patients with ruptured intraeranial aneurysms:arandomis-ed comparison of effects on survival,dependency,seizures,rebleeding,subgroups,and aneurysm occlusion[J].Lancet,2005,366(9 488):809-817.
[27] FRASER J F,RIINA H,MITRA N,et al.Treatment of ruptured intracranial aneurysms:looking to the past to register the future[J].Neurosurgery,2006,59(6):115-116.
[28] 王高强,徐文中.显微开颅夹闭术与血管内栓塞对颅内前循环动脉瘤患者的疗效比较[J].中国实用神经疾病杂志,2018,21(12):1 338-1 343.
[29] MRAK G,DURIC K S,NEMIR J,et al.Middle cerebral artery fusiform aneurysm presented with stroke and delayed subarachnoid hemorrhage trapping,hrombectomy,and bypass[J].Surg Neurol Int,2016,7(9):209-213.
[30] YANG K,AHN J S,PARK J C,et al.The efficacy of bypass surgery using a short interposition graft for the treatment of intracranial complex aneurysm[J].World Neurosurg,2015,83(2):197-202.
[31] DUBOVOY A V,OVSYANNIKOV K S,GUZHIN V E,et al.The use of high-flow extracranial-intracranial artery bypass in pathology of the cerebral and brachiocephalic arteries:technical features and surgical outcomes[J].Zh Vopr Neirokhir Im N N Burdenko,2017,81(2):5-21.
[32] 李敏,顾志强,周朋利,等.瘤颈栓塞治疗颅内动脉瘤破裂的单臂研究[J].中国实用神经疾病杂志,2018,21(14):1 530-1 536.
(收稿2018-08-30 修回2018-12-10)
本文责编:夏保军
本文引用信息:李彦钊,孙丕通,邓东风,孙晶,郎明非,曲晓扬,张绪新.巨大型颅内动脉瘤显微外科手术临床分析[J].中国实用神经疾病杂志,2018,21(24):2681-2685.DOI:10.12083/SYSJ.2018.24.560
Reference information:LI Yanzhao,SUN Pitong,DENG Dongfeng,SUN Jing,LANG Mingfei,QU Xiaoyang,ZHANG Xuxin.Clinical analysis of microsurgical treatment of giant intracranial aneurysms[J].Chinese Journal of Practical Nervous Diseases,2018,21(24):2681-2685.DOI:10.12083/SYSJ.2018.24.560