目的 分析成人视神经脊髓炎脑部影像表现及临床特点。方法 回顾分析2010-10—2017-10开封市中心医院收治的25例视神经脊髓炎患者为研究对象,并行头颅及脊髓MRI检查,根据头颅MRI检查结果,将有脑部病灶的患者纳入研究病例。结果 采用1.5T MR扫描仪对患者头部和脊髓进行检查获取MRI图像结果显示:25例患者中头部MRI检查中出现脑部病变者16例,未见出现脑部病变9例。病变主要位于延髓、脑桥、侧脑室周围、第三室周围、中脑导水管、胼胝体、大脑白质等处,根据病灶形态可分为斑片状、斑点状、线样状、
视神经脊髓炎脑部受累的MRI特征性影像表现及临床分析
张倩倩1) 张体华2) 周玫娟2) 钱伟军1)△
1)开封市中心医院影像科,河南 开封 475000 2)商丘医学高等专科学校,河南 商丘 476000
基金项目:河南省高等教育教学改革研究与实践项目(编号:2017SJGL649)
作者简介:张倩倩,Email:278440299@qq.com
△通信作者:钱伟军,Email:qwj1120714@foxmail.com
【摘要】 目的 分析成人视神经脊髓炎脑部影像表现及临床特点。方法 回顾分析2010-10—2017-10开封市中心医院收治的25例视神经脊髓炎患者为研究对象,并行头颅及脊髓MRI检查,根据头颅MRI检查结果,将有脑部病灶的患者纳入研究病例。结果 采用1.5T MR扫描仪对患者头部和脊髓进行检查获取MRI图像结果显示:25例患者中头部MRI检查中出现脑部病变者16例,未见出现脑部病变9例。病变主要位于延髓、脑桥、侧脑室周围、第三室周围、中脑导水管、胼胝体、大脑白质等处,根据病灶形态可分为斑片状、斑点状、线样状、融合型,不规则型,常见病灶为散在不规则斑片状、斑点状。15例患者MRI增强检查未见明显强化,1例患者病灶呈轻度强化。16例患者中均出现视神经和脊髓以外的中枢神经系统损害。结论 大多数视神经脊髓炎患者都会伴有脑部病变,绝大多数病灶部位与患者的临床表现具有对应关系,病变部位易伴发相应临床的表现。
【关键词】 视神经脊髓炎;脑部受累;磁共振成像;临床特点;脱髓鞘
【中图分类号】 R774.6 【文献标识码】 A 【文章编号】 1673-5110(2018)21-2367-06 DOI:10.12083/SYSJ.2018.21.507
MRI features and clinical analysis of brain involvement in optic neuromyelitis
ZHANG Qianqian1),ZHANG Tihua2),ZHOU Meijuan2),QIAN Weijun1)
1)Department of Imaging,Kaifeng Central Hospital,Kaifeng 475000,China;2)Shangqiu Medical College,Shangqiu 476000,China
【Abstract】 Objective Analysis of brain imaging features and clinical features of adult optic nerve myelitis.Methods From October 2010 to October 2017,25 cases of optic neuromyelitis treated in Kaifeng Central Hospital were retrospectively analyzed.The head and spinal cord MRI were performed.According to the results of cranial MRI,the patients with brain lesions were included in the study.Results The head and spinal cord of the patients were examined by 1.5T MR scanner.Of the 25 patients,16 had brain lesions in MRI examination,9 had no brain lesions.The lesions were mainly located in the medulla oblongata,pontine,lateral ventricle,and around the third ventricle.The midbrain aqueduct,corpus callosum,and white matter of the brain can be divided into patchy,speckled,linear,fused,multiple sclerosing,irregular,and irregular lesions according to the shape of the lesions.There was no obvious enhancement on MRI enhancement in 1 case.The optic nerve and the central nervous system outside the spinal cord were damaged in all of the 16 patients.Conclusion Most patients with optic nerve spondylitis have brain lesions,most of the lesions are associated with the clinical manifestations of the patients,and the lesions tend to accompany the clinical findings.
【Key words】 Optic neuromyelitis;Brain damage;MRI;Clinical characteristics;Demyelinate
视神经脊髓炎患者脑部病变的影像表及临床特征现仍在调查研究阶段,还没有明确的调查研究结果。因此,本次研究对2010-10—2017-10开封市中心医院收治的25例视神经脊髓炎患者的MR资料进行分析。
1 资料与方法
1.1 临床资料 回顾分析2010-10—2017-10开封市中心医院收治的25例视神经脊髓炎脑部受累者的MRI表现及临床特征,18例为视神经脊髓炎,7例为视神经脊髓炎高危综合征;25例患者均已确诊为视神经脊髓炎伴脑病变影像表现,其中男6例,女 19例,发病年龄18~63 (43.18±1.74)岁,病程3个月~6 a。所有病人均满足2015视神经脊髓炎诊断标准[1]:必备条件为视神经炎和横贯性脊髓炎,同时满足3项支持标准中的至少2项:(1)脊髓MRI 病灶累及范围大于3个脊椎节段;(2)颅脑MRI检查表现为正常或不符合多发性硬化诊断标准;(3)AQP4抗体为阳性。
1.2 方法 25例患者采用脊髓、头颅MRI进行影像学检查,采用东芝VANTAGE 1.5T MRI扫描仪进行MRI检查,脊髓扫描包括矢状位T1WI、T2WI、压脂像T2WI、横断T2WI;取仰卧位行头颅线圈快速SE序列扫描,扫描序列包括横轴位的T1WI、T2WI、FLAIR、DWI、ADC与矢状位T2WI,扫描参数T1WI:TR=2 000 ms,TE=15 ms;T2WI:TR=5 000 ms,TE=105 ms;FLAIR:TR=6 500 ms,TE=105 ms;DWI:TR=6 700 ms,TE=120 ms,b=0和1 000 mm2/s;厚度5.5 mm,螺旋距离间隔选择0 mm,应用GD-DTPA增强造影剂进行增强扫描。
2 结果
2.1 头颅影像表现 头颅影像检查诊断结果中25例患者检查结果异常者16例。16例患者的病灶分布部位如表1所示,病灶主要在脑室周围,包括侧脑室及三、四脑室;其次是大脑半球白质区。脑损害的16例患者中病灶呈对称者2例(12.5%)。MRI表现为病灶为T1WI等、低信号,T2WI呈高信号,FLAIR为高信号,DWI为等、低信号;增强扫描检结果示,16例脑部病灶出现轻度强化者1例(6.25%)。脑部病灶呈融合性2例(12.5%),呈散在不规则10例(62.5%),斑点状、线样、类圆形病变者4例(25.0%)。颅内病灶呈多为稍长T1或等T1信号影,呈长T2信号影,FLAIR序列呈高信号影,DWI呈稍高或等信号影,ADC呈等信号。1例融合性病灶见于胼胝体部,周围水肿明显,随访慢性期胼胝体常萎缩。2例延髓病灶位于延髓背侧。增强检查仅1例患者病灶呈轻度强化,15例均无不强化,这一点可与MS相鉴别。
2.2 临床特征 对照MRI未见出现脑部病变的患者,视神经脊髓炎脑部病变的患者起病方式分为急性起病和慢性起病,由于脑部大部分受累,按其临床表现分为:首发症状,脑干症状、小脑症状、脑部症状;首 发症状以视力突然下降为主,脑干症状以呕吐、顽固性呃逆、延髓功能障碍、视物旋转和复视,小脑症状表现为共济失调,脑部症状表现为嗜睡、昏迷、抽搐等。脑部损伤临床表现均颅内病灶的位置有直接联系。
3 讨论
视神经脊髓炎患者多累及脊髓神经与视神经,是一种特异性中枢神经系统炎性脱鞘性疾病,多见于育龄期女性,发病年龄34~43岁,女性与男性患者比例3:1~10:1,大部分视神经脊髓炎病人颅内受累。具有反复发作特征,致死率、致残率很高,视神经脊髓炎是多发性硬化变异型的一种,还是一种独立的形态存在,临床争议较大[2-3]。由于视神经脊髓炎和多发性硬化临床表现存在较大的重叠,所以鉴别较为困难。根据相关文献[4-14]报道,视神经脊髓炎的病理生理过程和免疫机制与多发性硬化存在较大不同,影像表现略有不同,同时临床诊疗方法也存在差异,因此,临床治疗过程中视神经脊髓炎患者的早期鉴别诊断具有重要临床意义。
本次研究中25例视神经脊髓炎患者中16例出现脑部异常,占64%,与国外研究一致[15-20],而国内报告视神经脊髓炎伴脑损害者高达80%,结合国内外研究可知,临床治疗过程中视神经脊髓炎伴脑部损伤较为常见。从病灶部位而言,MRI检查示病变主要位于延髓、脑桥、侧脑室周围、第三室周围、中脑导水管、胼胝体、大脑白质处及皮质下,皮质未见受累。根据病灶形态可分为斑片状、斑点状、线样状、融合型、不规则型,常见病灶为散在不规则斑片状、斑点状稍长T1或等T1信号影,T2WI及FLAIR序列呈高信号影,DWI呈稍高或等信号影,ADC呈等信号。本次研究表明,散在不规则病灶占70%,远超过其他病灶形态,病灶除主要分布在侧脑室、中脑导水管及三、四脑室周围AQP高表达区外,其次是大脑白质区,皮质未见病灶(图1~2)。2例随访病例脑内病灶随着时间推移病灶有逐渐增多的特点。视神经脊髓炎脑部增强绝大多数不强化(图3)。有研究认为,视神经脊髓炎急性期除脊髓病灶可出现强化外,脑部病灶也可出现云雾样、铅笔芯样、软脑膜强化[21-25]。视神经脊髓炎患者主要与多发性硬化患者进行鉴别,二者主要病灶位置存在差异;其次,NMO患者头部MRI未出现皮质病灶及脑萎缩,而多发性硬化在早期阶段也多见皮质病灶与萎缩[26-31]。
本文通过分析NMO的颅脑常规MRI特征,结合脊髓MRI检查及视神经检查有助于提高对NMO的认识及早期诊断率,早期有效治疗能降低复发率和致残率。
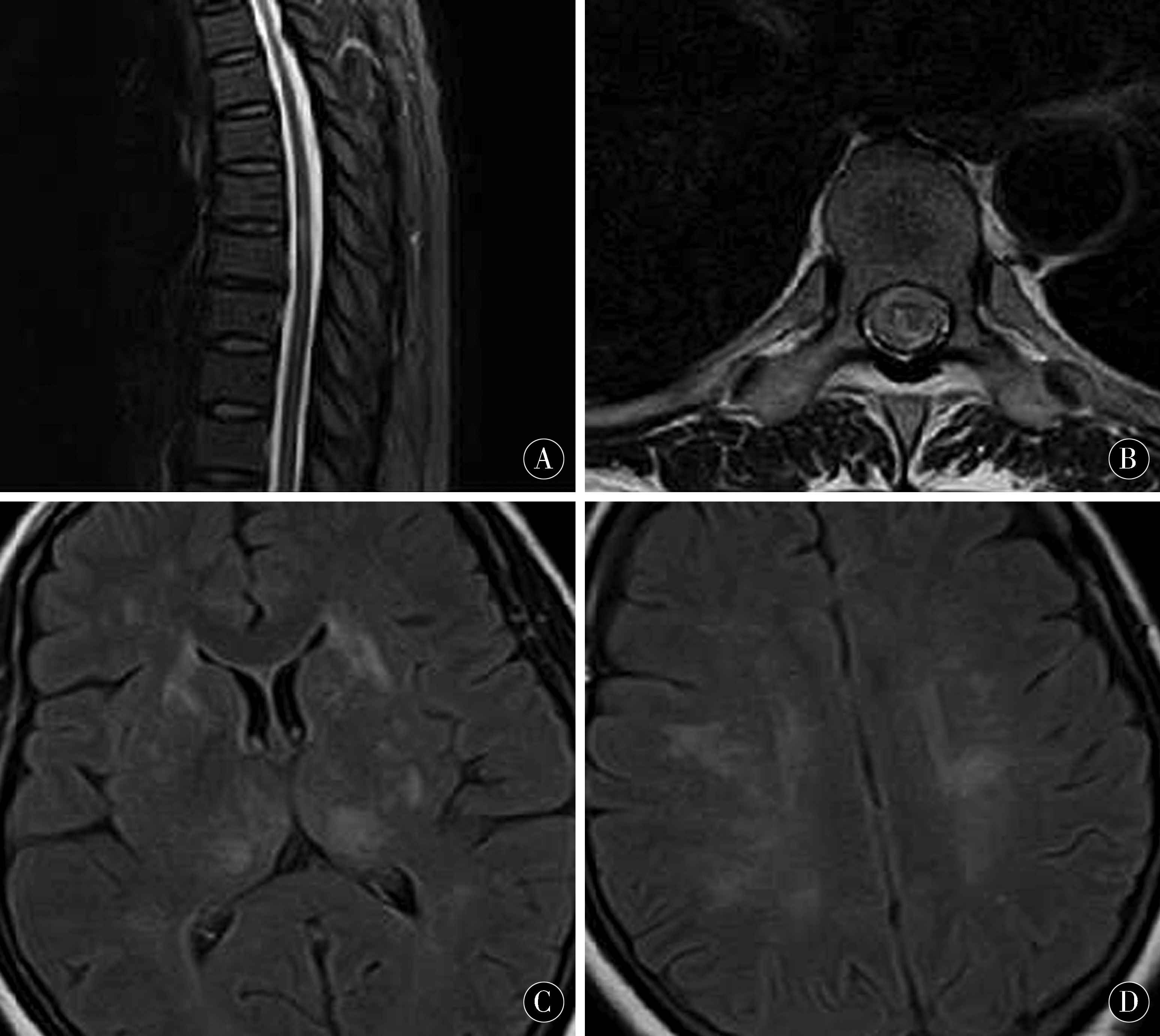
图1 矢状T2压脂及T2横断位胸髓内线样、斑点状信号影;FLAIR序列示双侧丘脑、大脑半球白质区多发斑点状高信号
Figure 1 Sagittal T2 compression and T2 transverse thoracic intramedullary,speckle signal intensity;FLAIR sequence:bilateral thalamus,multiple speckle hyperintense in the white matter area of the cerebral hemisphere
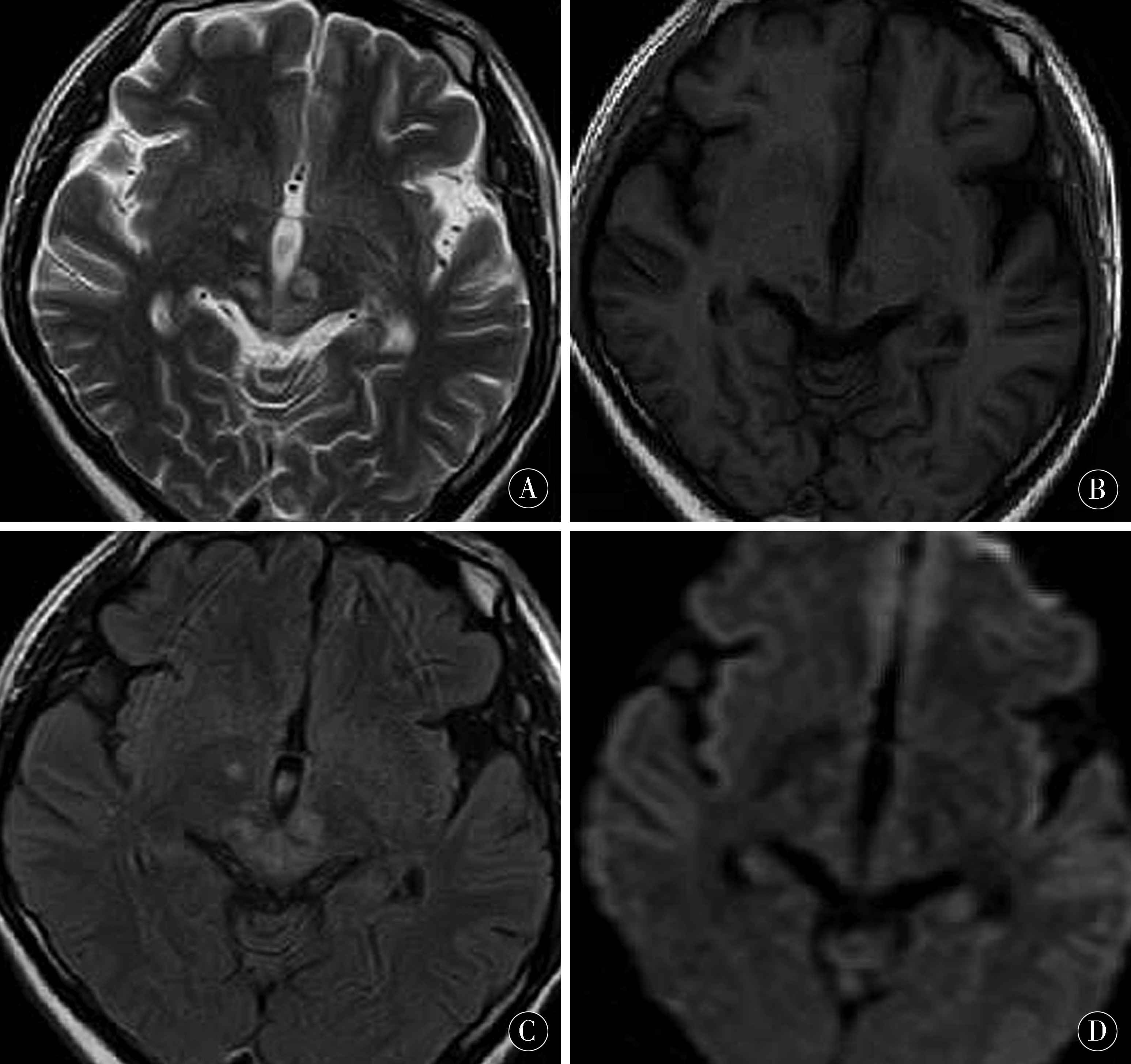
图2 中脑、丘脑斑片状、斑点状长T1、T2信号影,DWI呈略高信号,FLAIR像高信号影
Figure 2 Mesencephalon,thalamic plaques, speckled long T1,T2 signal intensity,DWI was slightly hyperintense,FLAIR image was hyperintense
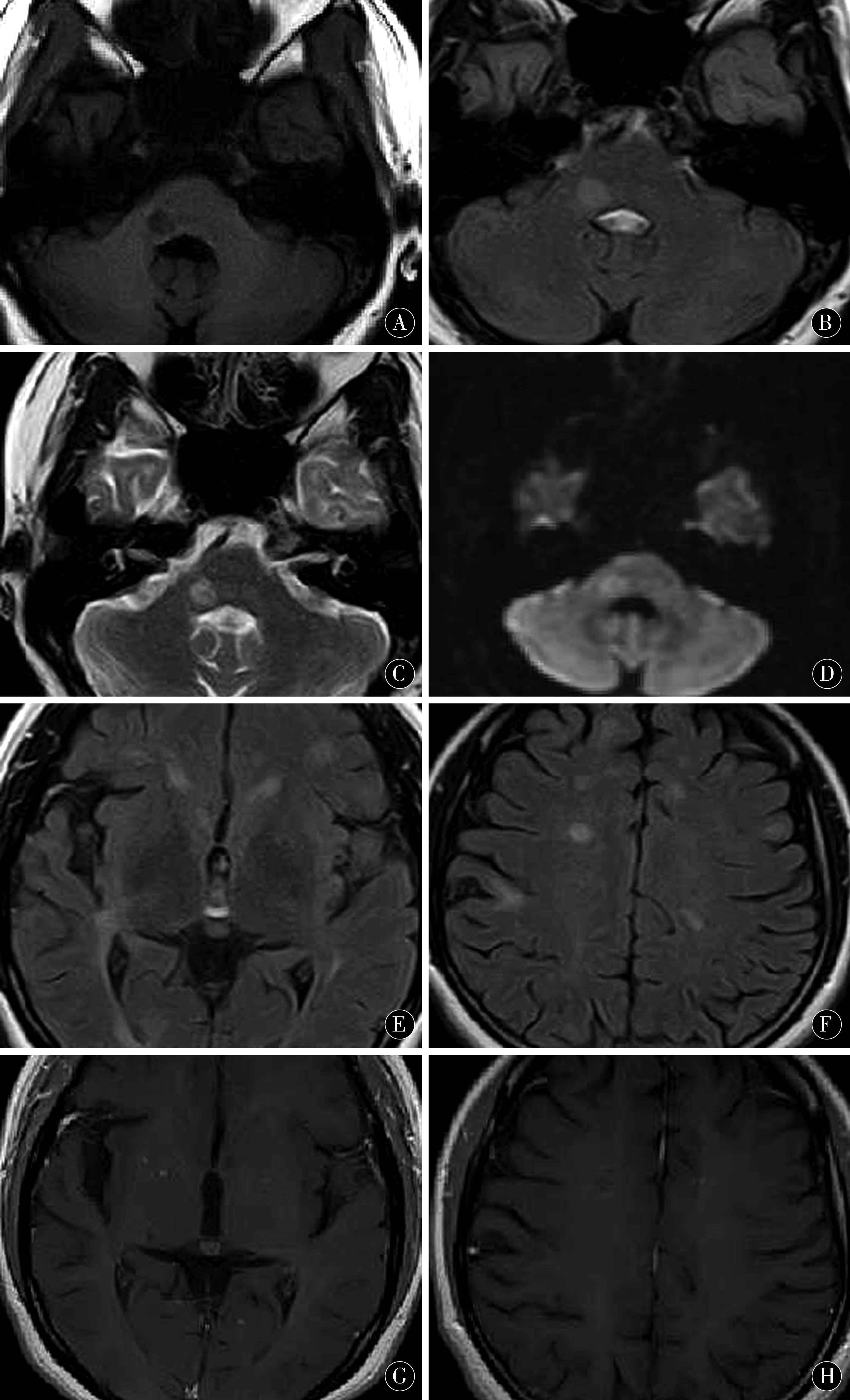
图3 脑桥、双侧大脑半球白质内、侧脑室周围多发斑点状、斑片状长T1、T2信号影,DWI呈略高信号,FLAIR像呈高信号,增强无强化
Figure 3 Pontine,bilateral cerebral hemispheric white matter,multiple spots around the lateral ventricle,patchy long T1 T 2 signal intensity,DWI showed slightly high signal intensity,FLAIR image showed high signal intensity,enhancement without reinforcement
表1 16例患者病灶位置 [n(%)]
Table 1 Location of lesions in 16 patients [n(%)]
| 病灶分布 |
n |
| 大脑半球白质 |
4(25.0) |
| 胼胝体 |
2(12.5) |
| 侧脑室周围 |
7(43.7) |
| 中脑导水管周围 |
2(12.5) |
| 第三、四室周围 |
4(25.0) |
| 脑桥 |
3(18.7) |
| 延髓 |
2(12.5) |
4 参考文献
[1] WINGERCHUK D M,BANWELL B,BENNETT J L,et al.International consensus diagnostic criteria for neuromyelitis optica spectrum Disorders[J].Neurology,2015,85(2):177-189.
[2] AUNASUMART S,APIWATTANAKUL M.Clinical outcomes and predictive factors related to Good outcomes in plasma exchange in severe attack of NMOSD and long extensive transverse myelitis:case series and review of the literature[J].Mult Scler Relat Disord,2017,13(1):93-97.
[3] LIU Y,WANG J,DAAMS M et al.Differential patterns of spinal cord and brain atrophy in NMO and MS[J].Neurology,2015,84(14):1 465-1 472.
[4] OCHI H,FUJIHARA K.Demyelinating diseases in Asia[J].Curr Opin Neurol,2016.29(3):222-228.
[5] HOR J Y,LIM T T,CHIA Y K.et al.Prevalence of neuromyelitis optica spectrum disorder in the multi-ethnic Penana Island,Malaysia,and a review of worldwide prevalence [J].Mult Scler Relat Disord,2017,19(1):20-24.
[6] SUN H,SUN X,LI J,et al.Gender differences among Chinese pabents with neuromyelitis optica spectrum disorders [J].Mult Scler Relat Disord,2017,17 (1):5-8.
[7] EIZAA RIRRE M B,ALONSO R,VANOTTI S.et al.Cognitive impairment in neuromyelitis optica spectrum disorders:what do we know? [J].Mult Scler Relat Disord,2017,18:225-229.
[8] SAHRAIAN M A,MOAHADASI A N,AZIMI A R,et al.Diagnosis and rnanaaement of neuromyelitis optica spectrum disorder(NMOSD) in Iran:a consensus a rideline and recommendations [J].Mult Scler Relat Disord,2017,18:144-151.
[9] KESSLER R A,MEALY M A,JIMENEZ-ARANAO J A,et al.Anti-aqrra-porin-4 titer is not predictive of disease course in neuromyelitis optica spectrum disorder:a multicenter cohort study [J].Mult cler Relat Disord,2017,17:198-201.
[10] SATO D K,CALLEAARO D,LANAPEIXOTO M A.et al.Distinction between MOG antibody-positive and AQP4 antibody-positive NMO spectrum disorders [J].Neurolony,2014,82 (6 ):474-481.
[11] PUNDIT L,SATO D K,MUSTAFA S.Serological markers associated with neuromyelitis optica spectrum disorders in South India [J].Ann Indian Acad Neuro1,2016,19(4):505-509.
[12] PACHE F,ZIMMERMANN H,FINKE C,et al.Brain parenchymal damage in neuromyelitis optica spectrum disordet-A multimodal MRI study[J].Eur Radiol,2016,26(12):4 413-4 422.
[13] DERLE E,GIINES HN,KONUSKAN B,et al.Neuromyelitis optiea in children:a review of the literature[J].Turk J Pediatr,2014,56(6):573-580.
[14] PLAUBORG A V,HANSEN AV AND GARNE E.Use of azathioprine and corticosteroids during pregnan-cy and birth outcome in women diagnosed with inflammatory bowel disease[J].Birth Defects Res A Clin Mol Teratol,2016,106(6):494-499.
[15] 李娇,高秀丽.水通道蛋白4抗体的研究发展[J].中国实用神经疾病杂志,2018,21(13):1 499-1 504.
[16] FRANCIOTTA D,GASTALDI M,SALA A,et al.Diagnostics of the neuromyelitisoptica spectrum disorders (NMOSD)「J].Neurol Sci,2017,38:231-236.
[17] LIU J,ZHANG Q,LIAN Z,et al.Painful tonic spasm in neuromyelitisoptica spectrum disorders:Prevalence,clinical implications and treatment options「J].Mult Scler Relat Disord,2017,17:99-102.
[18] CARNERO CONTENTTI E,LEGUIZAMON F,HRYB J P,et al.Neuromyelitisoptica:association with paroxysmal painful tonic spasms[J].Neurologia,2016,31:511-515.
[19] VON GLEHN F,JARIUS S,C'AVALCANTI LIRA RP,et al.Structural brain abnorm-alities are related to retinal nerve fiber layer thinning and disease duration in neuromyelitis optica spectrum disorders[J].Mult Scler,2014,20(9):1 189-1 197.
[20] JUREWICZ A,SELINAJ K.Relapse of neuromyelitis optica during pregnancy -treahnent options and literatu-re review [J].Clin Neurol Neurosurg,2015,130:159-161.
[21] DAVOUDI V,KEYHANIAN K,BOVE R M,et al.Immunology of neuromyelitis optica during pregnancy [J].Neurol Neuroimmunol Neuroinflamm,2016,3(6):e288.
[22] NOUR M M NAKASHIMA I,COUTINHO E,et al.Pregnancy outcomes in aquaporin -4-positive neuromyelitis optica spectrum disorder [J]Neurology,2016,86(1):79-87.
[23] RUBIO TABARES J,AMAYA GONZALEZ P F.Plasma exchange therapy for severe relapse of Devic's disease in a pregnant woman:A case report andconcise review [J].Clin Neurol Neurosurg,2016,148:88-90.
[24] HOH J H,HO H S,LEE J,et al.Pregnany and patients with preexisting lupus nephritis:15 years of experience at a single center in Korea [J]Lupus,2015,24(7):764-772.
[25] PONTICELLI C AND MORONI G.Immunosuppre-ssion in pregnant women with systemic lupus erythematosus[J].Expert Rev Clin &nmunol,2015,11(5):549-552.
[26] LONG Y,CHEN M,ZHANG B.et al.Brain gado-linium enhancement along the ventricular and leptomeningeal regions in patients with aquaporin-4 antibodies in cerebral spinal fluid[J].J Neuroimmunol,2014,269(1-2):62-67.
[27] ZALEWSKI N L,MORRIS P P,WEINSHENKER B G,et al.Ring-enhancing spinal cord lesions in spinal cord lesion in neuromyelitis optica spectrum disorders.J Neurol Neurosurg Psychiatry,2017,88(3):218-222.
[28] LIU Y,WANG J,DAAMS M,et al.Differential patt-erns of spinal cord and brain atrophy in NMO and MS[J].Neurology,2015,84(14):1 465-1 472.
[29] JEONG I H,CHOI J Y,KIM S H,et al.Normal-appearing white matter demyelinationin neuromyelitis optica spectrum disorder[J].Eur J Neurol,2017,24(4):652-658.
[30] OCHI H,FUJIHARA K.Demyelinating diseases in Asia[J].Curr Opin Neurol,2016,29(3):222-228.
[31] PEKCEVIK Y,MITCHELL CH,MEAY MA,etal.differentiating neuromyelitis optica from other causes of longitudinally extensive transverse myelitis on spinal magnetic resonance imaging [J].Mult Scler,2016,22(3):302-311.
(收稿2018-09-22 修回2018-10-30)
本文责编:关慧
本文引用信息:张倩倩,张体华,周玫娟,钱伟军.视神经脊髓炎脑部受累的MRI特征性影像表现及临床分析[J].中国实用神经疾病杂志,2018,21(21):2367-2372.DOI:10.12083/SYSJ.2018.21.507
Reference information:ZHANG Qianqian,ZHANG Tihua,ZHOU Meijuan,QIAN Weijun.MRI features and clinical analysis of brain involvement in optic neuromyelitis[J].Chinese Journal of Practical Nervous Diseases,2018,21(21):2367-2372.DOI:10.12083/SYSJ.2018.21.507