目的 研究磁共振对视神经脊髓炎谱系疾病患者的诊断价值。方法 收集临床诊断为NMOSD的12例患者行颅脑MRI轴位T1WI、T2WI、T2WI-FLAIR,矢状位T2WI序列,冠状位眼眶STIR序列,颈胸段脊髓的矢状位T1WI、T2WI及STIR序列,轴位T2WI序列扫描,其中5例进行增强扫描,分析颅内、视神经及脊髓内病变累及的部位及范围。结果 12例患者均出现脑内典型部位的多发病灶,单侧或双侧视神经病变;8例出现脊髓内病灶,增强扫描5例患者中4例脑内部分病灶见强化,4例有视神经强化,3例脊髓内病灶局部可见强化。结论 MRI平扫及增强扫描对NMOSD患者有非常高的诊断价值,可以对疾病作出早期诊断,对疾病分期、疗效评价及预后有一定的诊断价值。
磁共振对视神经脊髓炎谱系疾病的诊断价值研究
杨 靖 周 军 黄立新
沈阳市第四人民医院放射科,辽宁 沈阳 110031
作者简介:杨靖,Email:yangjingst@163.com
【摘要】 目的 研究磁共振对视神经脊髓炎谱系疾病患者的诊断价值。方法 收集临床诊断为NMOSD的12例患者行颅脑MRI轴位T1WI、T2WI、T2WI-FLAIR,矢状位T2WI序列,冠状位眼眶STIR序列,颈胸段脊髓的矢状位T1WI、T2WI及STIR序列,轴位T2WI序列扫描,其中5例进行增强扫描,分析颅内、视神经及脊髓内病变累及的部位及范围。结果 12例患者均出现脑内典型部位的多发病灶,单侧或双侧视神经病变;8例出现脊髓内病灶,增强扫描5例患者中4例脑内部分病灶见强化,4例有视神经强化,3例脊髓内病灶局部可见强化。结论 MRI平扫及增强扫描对NMOSD患者有非常高的诊断价值,可以对疾病作出早期诊断,对疾病分期、疗效评价及预后有一定的诊断价值。
【关键词】 视神经脊髓炎;视神经脊髓炎谱系疾病;磁共振成像;液体抑制反转恢序列;脂肪抑制
【中图分类号】 R745 【文献标识码】 A 【文章编号】 1673-5110(2018)24-2697-06 DOI:10.12083/SYSJ.2018.24.563
The value of magnetic resonance imaging in the diagnosis of optic neuromyelitis spectrum disease
YANG Jing,ZHOU Jun,HUANG Lixin
Fourth People's Hospital of Shenyang,Shenyang 110031,China
【Abstract】 Objective To study the value of magnetic resonance imaging in the diagnosis of patients with optic neuromyelitis spectrum disease.Methods Twelve patients with clinical diagnosis of NMOSD were enrolled in the MRI axial T1WI,T2WI,T2WI-FLAIR,sagittal T2WI sequence,coronal STIR sequence,sagittal T1WI,T2WI and STIR sequences of the cervical and thoracic spinal cord.Axial T2WI sequence scans,5 of which were enhanced scans.The location and extent of lesions in the intracranial,optic and spinal cords of these patients were analyzed.Results Twelve patients had multiple lesions in the typical part of the brain,unilateral or bilateral optic neuropathy,8 patients had intraspinal lesions,and 4 patients in the enhanced scan showed enhancement of brain lesions in 4 patients,4 patients There were optic nerve enhancement,and the lesions in the spinal cord of 3 patients were locally enhanced.Conclusion MRI plain scan and enhanced scan have very high diagnostic value for NMOSD patients,can make early diagnosis of disease,and have certain diagnostic value for disease staging,post-treatment efficacy evaluation and prognosis.Therefore,magnetic resonance examination is NMOSD.The necessary examination means for the patient.
【Key words】 Neuromyelitis optica;Neuromyelitis optica spectrum disorders;Magnetic resonance imaging;Fluid attenuated inversion recovery;Short T1 inversion recovery
视神经脊髓炎(neuromyelitis optica,NMO)是一组免疫相关的以中枢神经系统受累发病的急性或亚急性炎性脱髓鞘类疾病,这组疾病最早认识之初是以双侧视神经炎与脊髓炎同时发病为诊断特征,又称Devic病。随着近几十年医学的发展,特别是实验室、免疫学、影像学及病理学的不断研究和发展,对这组疾病的认识也不断深入,因此,2015-06国际NMO诊断小组对NMO一类疾病进行重新修订,应用视神经脊髓炎疾病谱系疾病(NMO spectrum disorders,NMOSD)作为这类疾病的统一术语,根据实验室血清学水通道蛋白-4(AQP-4)-IgG检验的结果分为阳性组和阴性组制定更加详尽的诊断标准[1-3]。新的诊断标准中基于血清学检查AQP4-IgG和临床发病特征为基础,进一步根据是否伴有视神经炎、长节段横贯性脊髓炎、脑内特征病变(最后区综合征、脑干综合征、间脑病灶等)作为NMOSD的诊断依据。磁共振是视神经、脊髓及颅内病变的检出及诊断的有效手段。本研究通过回顾分析12例经临床最终确诊的NMOSD患者的磁共振检查,分析磁共振对NMOSD患者的诊断价值。
1 资料与方法
1.1 研究对象 收集2014-06—2018-10来沈阳市第四人民医院检查,并最终经临床根据2015年修订标准诊断为NMOSD的12例患者为研究对象,所有患者以眼科症状为首诊,其中5例单侧视神经发病,7例双侧视神经异常(2例累及视交叉、视束),均进行眼科相关检查。其中男4例,女8例,发病年龄17~44岁,平均29.4岁。
1.2 磁共振扫描序列及参数 应用GE Signa HDx 1.5T 磁共振扫描仪进行扫描,8通道头线圈,8通道椎体线圈。颅脑MRI轴位T1WI、T2WI、T2WI-FLAIR,扫描层厚5.0 mm/层间距1.5 mm,矢状位T2WI序列扫描,扫描层厚6.0 mm/层间距1.0 mm,视神经采用冠状位STIR序列扫描,扫描范围从眼球后部-颅内视束,扫描层厚3.0 mm/层间距0.5 mm。颈胸段脊髓扫描矢状位T1WI、T2WI及STIR序列,扫描层厚4.0 mm/层间距0.5 mm,轴位T2WI序列扫描,扫描层厚3.0 mm/层间距0.5 mm。其中5例进行颅脑及脊髓的增强扫描,静脉注射GD-DTPA后行T1WI序列增强扫描。
1.3 影像分析 诊断阅片由2名副主任医师以上的放射科诊断医生采用双盲法完成。随机对12例NMOSD患者的颅脑、视神经及脊髓的磁共振图像分别读片,分析颅脑、视神经及脊髓内病变的部位、形态、范围、病灶的数量、信号强度等,5例增强扫描的患者对比分析增强前后有无强化,强化的范围、信号强度等,最后将会诊意见作为磁共振的最终检查结果。
2 结果
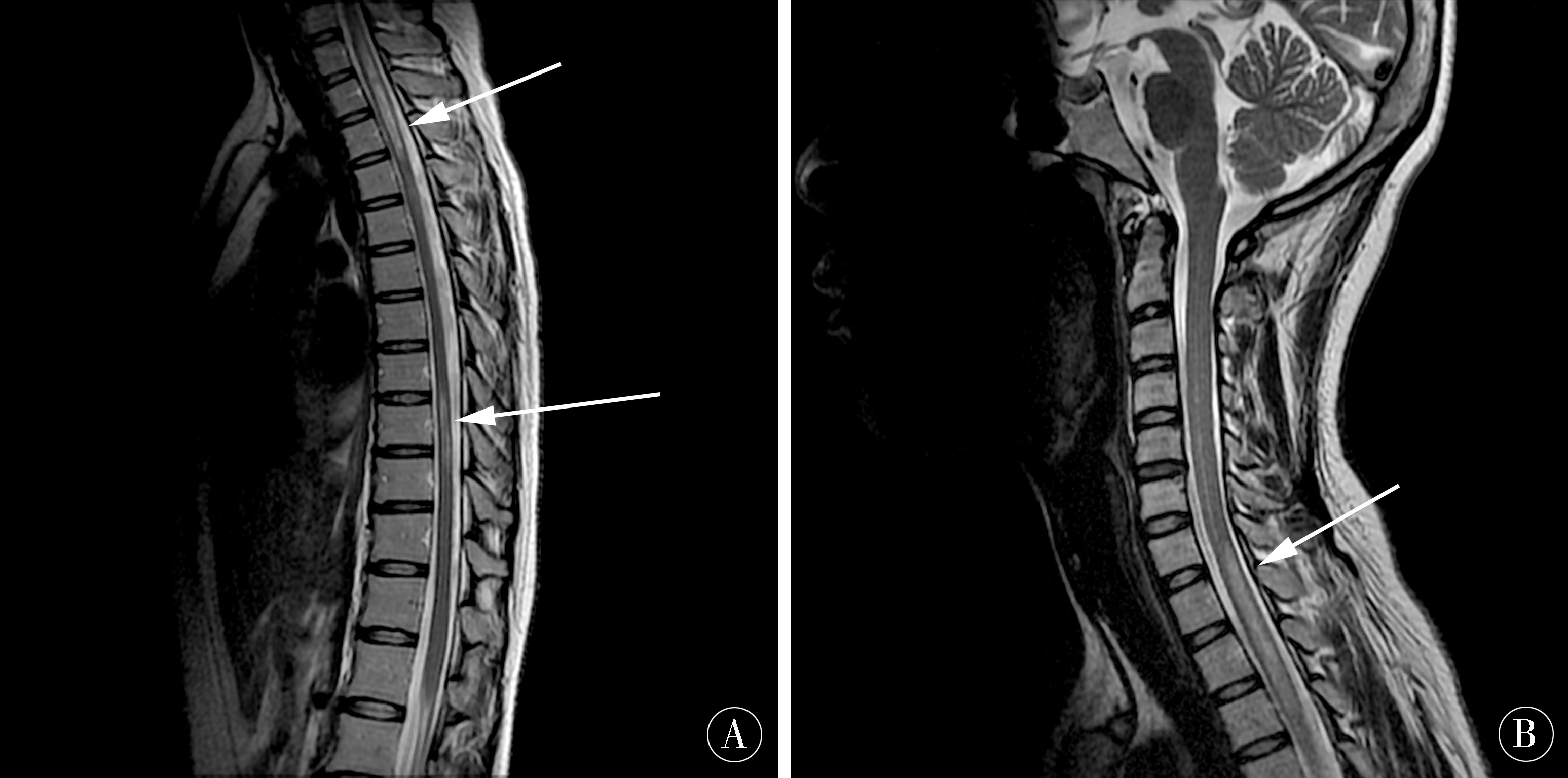
12例NMOSD患者颅脑、视神经及脊髓的磁共振检查图像与临床诊断结果进行比较,其中5例出现单侧视神经病变(4例出现单侧眶内段视神经炎改变,1例单侧视神经萎缩),7例双侧视神经出现病变,其中6例双侧视神经炎改变(3例病变范围为眶内段,1例病变范围眶内段及视神经管内段,2例病变范围较大累及视神经颅内段、视交叉及视束),还有1例左侧视神经萎缩,右侧视神经炎改变。12例NMOSD患者的颅内扫描病灶均是多发,部位多出现在双侧侧脑室、三脑室及第四的脑室旁室管膜下、下丘脑、脑干(中脑、脑桥、延髓)背侧,2例出现双侧皮质脊髓束至双侧大脑脚。12例患者的脊髓扫描范围以颈段和胸段脊髓为主,其中8例出现颈胸段脊髓的多发病灶,病灶多发为长节段的横贯性脊髓炎,4例出现颈段或胸段脊髓的单发病灶,2例病灶节长度1~2个椎体节段,2例>2个椎体节段。5例增强扫描患者中,4例出现颅内、视神经内病灶的部分强化,3例出现脊髓内病灶的强化。
3 讨论
视神经脊髓炎(NMO)是一种中枢神经系统的炎性脱髓鞘性疾病。近几年随着发病率的增高及检查手段的不断完善,这类疾病越来越多地被临床医生所认识,特别是在2015年国际NMO诊断小组对视神经脊髓炎疾病谱系疾病(NMOSD)这一概念的提出,更加完善了对这类疾病的认识,从临床表现、诊断标准都有了更新的认识,但发病原因还不明确,有研究表明与免疫反应、病毒感染以及遗传等因素相[4-6]关。本研究收集的12例患者中多数以眼科视力下降来诊,眼科为首诊科室,且发病时间以春秋两季伴病毒感染的病例数居多,年轻患者多发,女性多见。起病急、进展快,多数在发病1周左右来诊,出现视力的快速下降、视物不清[7],部分患者有过反复发作史,也有患者双眼不是同时发病,曾累及一侧视神经,又以另一侧视神经发病来诊,发现情况多样。根据累及颅内、脊髓病变的部位、病灶的数量的不同[8-9],临床表现也多样。但共同特点是发病急、症状重、进展快,临床预后较差[10-12]。因此,如何早期作出准确的诊断,选择准确、有效的治疗方法,是提高NMOSD患者预后的关键。
视神经脊髓炎疾病谱系疾病是针对血清学AQP4-IgG阳性和阴性的患者作出不同的诊断标准。对于AQP4-IgG阳性患者诊断更加简化,对于血清学AQP4-IgG阴性患者,提出了更加系统、明确的诊断标准。通过影像学尤其磁共振对于颅脑、视神经及脊髓内病灶的部位、数量都有详细的要求,对于AQP4-IgG阴性患者也能够早期作出明确诊断[13-15]。本研究中2例为2015年前AQP4-IgG阳性患者,诊断较明确,其余10例为2015年后采用NMOSD新的诊断标准进行诊断的患者,其中3例血清学AQP4-IgG阴性患者采用2015年新的NMOSD诊断标准后[16],诊断更加明确,检出率更高,对治疗和预后都很有帮助。
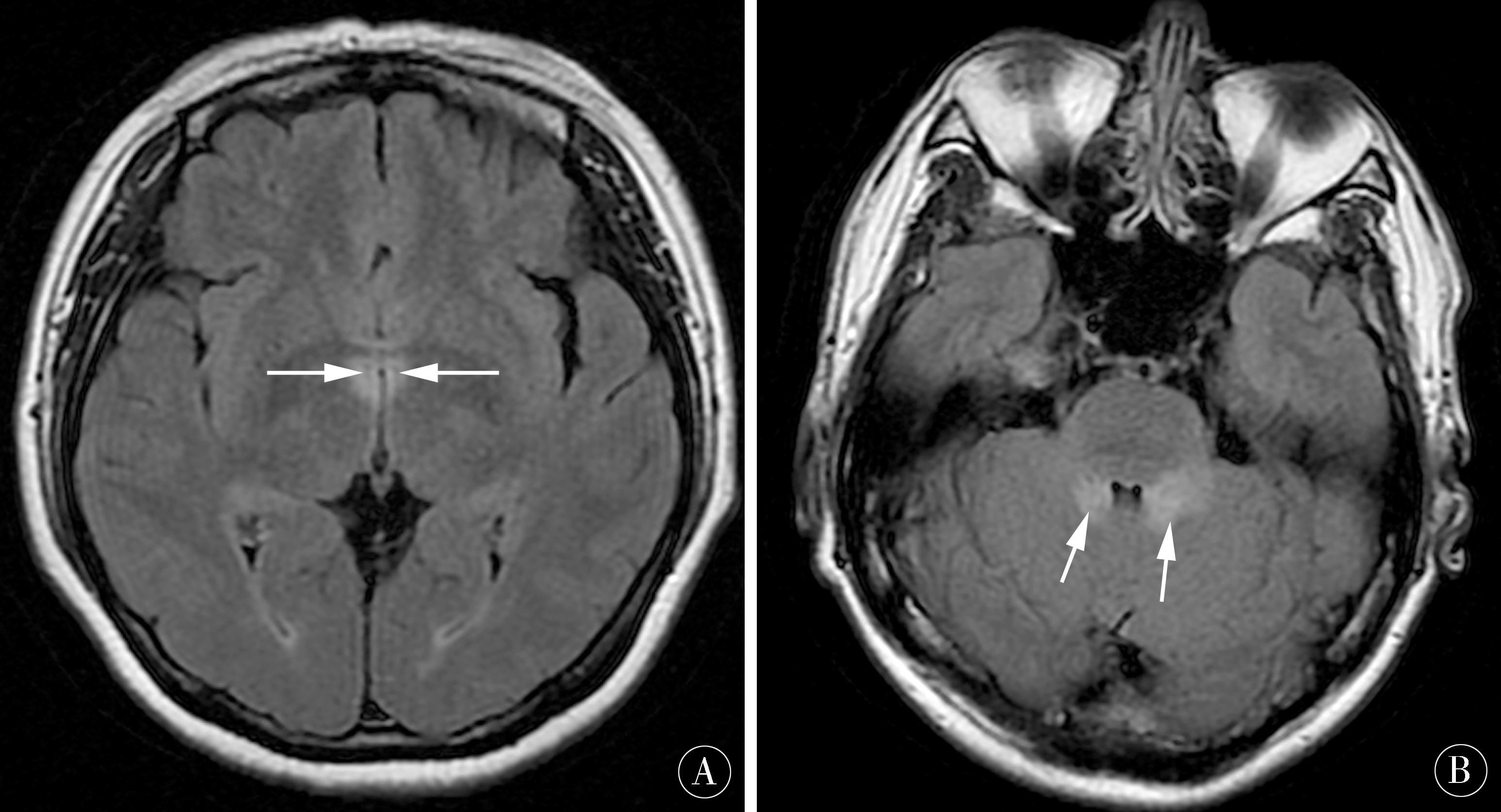
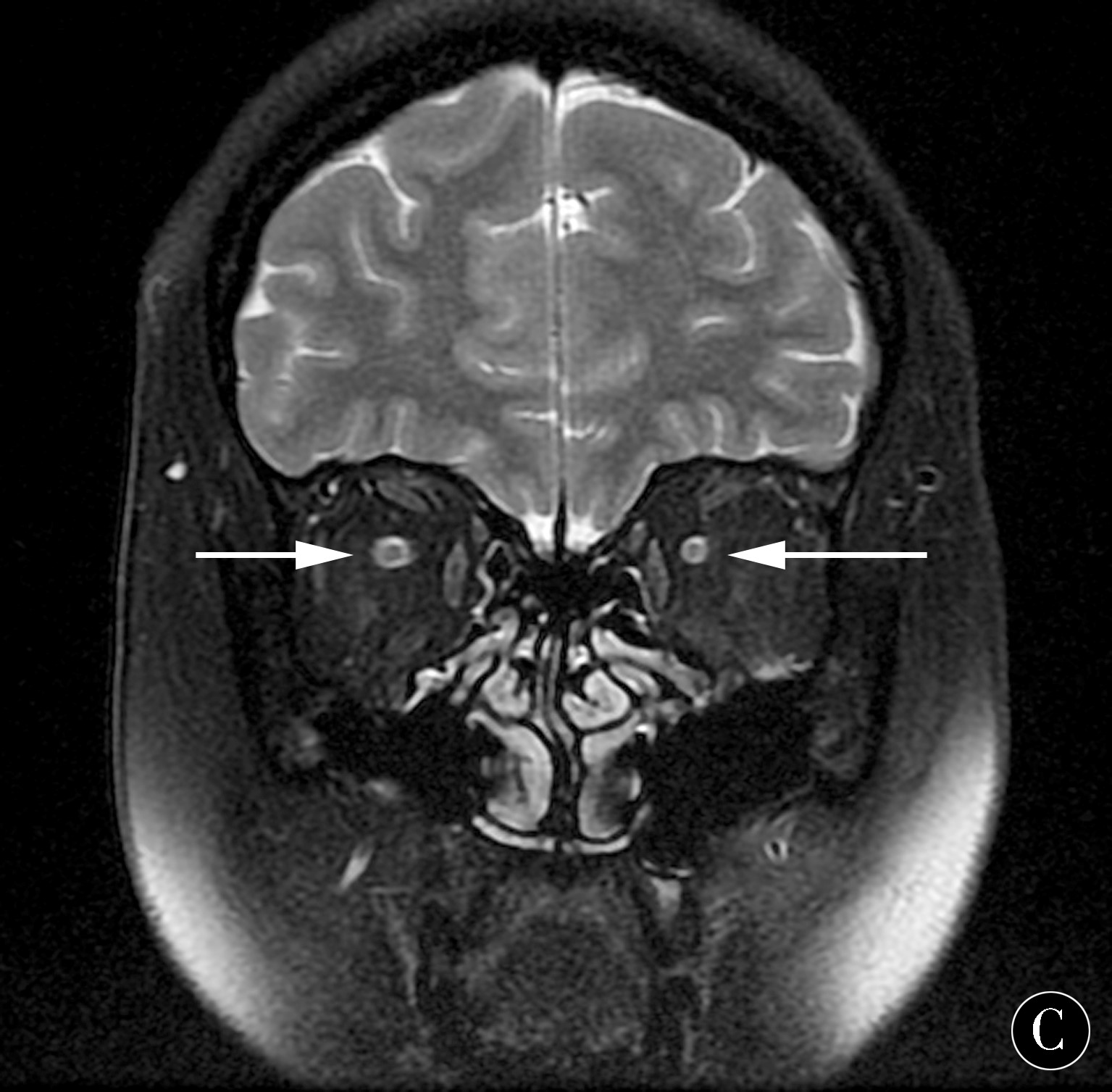
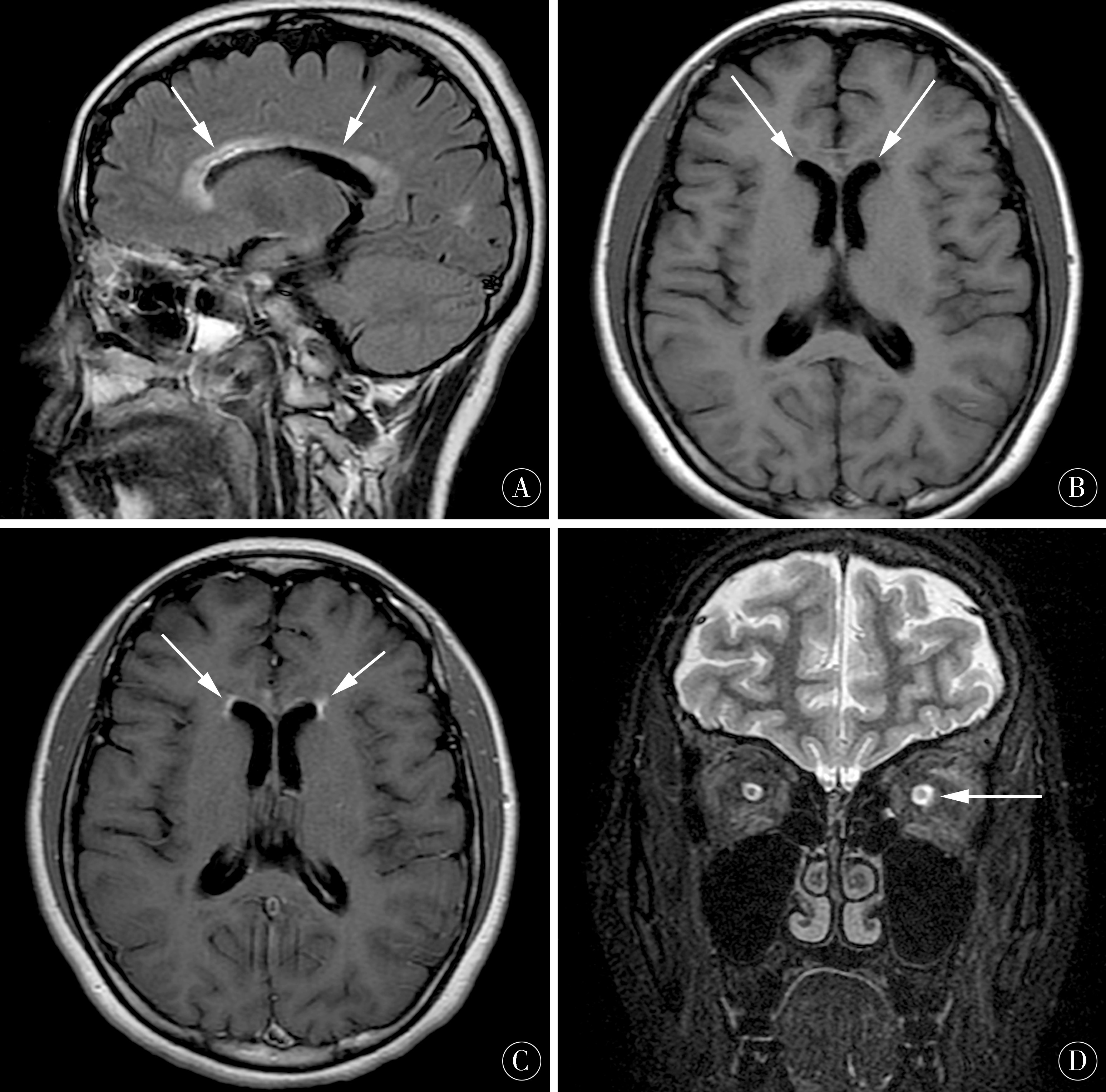
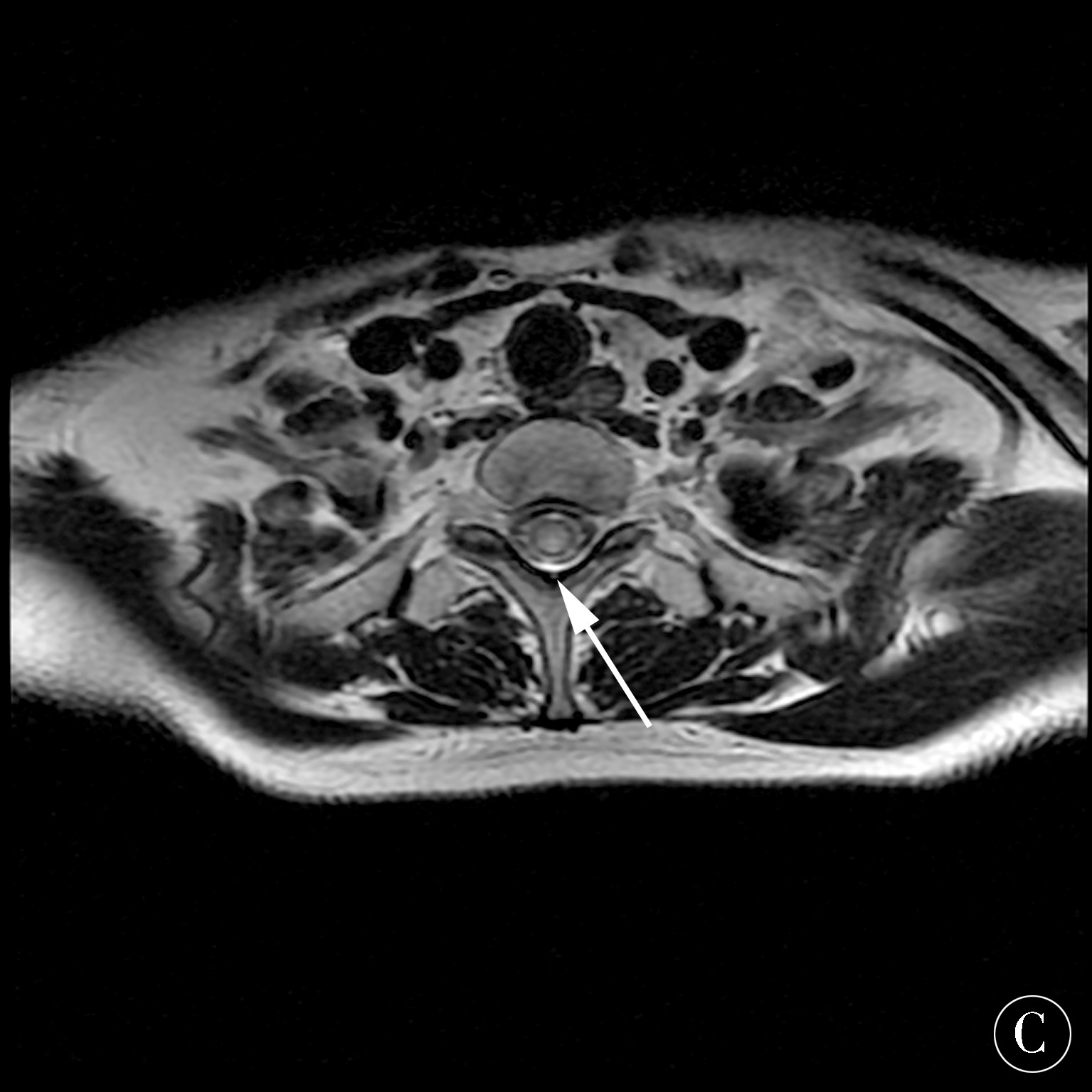
本研究中收集的12例NMOSD患者,均以眼科症状为首诊。沈阳市第四人民医院针对眼科视力下降、可疑视神经炎患者制定了专门的磁共振检查方案,首先,排除颅内炎性脱髓鞘疾病,明确视神经有无病变,选择以颅脑检查为主,排除颅内炎性脱髓鞘性疾病、视中枢的血管源性疾病、占位,以及鞍区病变;其次,做冠状位STIR或T2WI脂肪抑制序列,甚至三维冠状位视神经T2WI脂肪以及水抑制序列,明确视神经眶内段、管内段、颅内段、视交叉及视束有无病变[17-19]。12例患者的视神经累及范围较长,且视神经增粗明显,可以作出视神经炎的明确诊断,病例中双侧较多,也有单侧发病,部分病例有单侧视神经炎史,已出现既往患侧的视神经萎缩,又以另一侧视神经炎发病,符合NMOSD反复发作的特点[20-23]。本研究中病例1颅内病变明显累及第三脑室及第四脑室周围室管膜区域(图1A~B),同时伴双侧视神经明显增粗、视神经炎改变(图1C)。病例2颅内病变以双侧侧脑室周围室管膜下受累为主(图2A~C),增强扫描侧脑室周围部分病灶可见强化(图2C),同时伴左侧视神经炎改变(图2D)。12例NMOSD患者做了颈段和胸段脊髓的扫描,病灶多数是长节段的横贯性脊髓炎,有少数病例脊髓受累节段小于2个椎体节段(图3A~C)。但结合血清学检查、颅内和视神经病变,也可以作出视神经脊髓炎的诊断。5例做颅脑、视神经及脊髓的增强扫描发现,颅脑、视神经和脊髓的部分病灶出现强化,部分颅内病灶未见强化,2例视神经呈现轻度、模糊强化,分析原因可能与发病时间或反复发病相关[24-26]。
对于视神经脊髓炎疾病谱系疾病患者,磁共振检查是非常必要的手段,结合血清学AQP4-IgG以及临床眼科、神经科的典型发病症状可以作出明确诊断,特别是对血清学AQP4-IgG阴性患者,磁共振检查的意义更加重要[27-28]。根据新的诊断标准,也可以作出明确、早期诊断,同时磁共振也是预后随访评价的有效手段,平扫结合增强扫描对预后及病灶的评价有重要的临床意义,是患者必不可少的随访手段[29-30]。
图1 26岁女性患者,双眼视力下降5 d来诊A:T2WI-FLAIR序列,轴位可见第三脑室周围见信号增高(如箭头所示);B:脑干后部第四脑室周围见斑片状高信号影(如箭头所示);C:冠状位STIR序列双侧视神经增粗,信号增高,视神经炎改变
Figure 1 In a 26-year-old female patient,the vision of both eyes decreased for 5 days A:T2WI-FLAIR sequence,the axial position shows an increase in signal around the third ventricle (as indicated by the arrow);B:The posterior fourth ventricle around the brainstem sees a patchy high signal (such as the arrow);C:Coronal STIR sequence bilateral optic nerve thickening,increased signal,optic neuritis changes
图2 22岁女性患者,左眼视力下降1周来诊 A:矢状位 T2WI-FLAIR序列可见侧脑室旁及室管膜侠见点线状、斑条状高信号影(如箭头所示);B、C:轴位T1WI平扫及增强扫描序列可见双侧脑室前角旁室管膜下见线状强化(如箭头所示);D:冠状位STIR序列可见患者左侧视神经增粗、信号增高,视神经炎改变
Figure 2 22-year-old female patient with left eye vision decreased for 1 week A:Sagittal T2WI-FLAIR sequence shows visible lateral ventricle and ependyma,line-like,plaque-like high-signal shadow (indicated by the arrow);B-C:Axial T1WI plain scan and enhanced scan sequence show bilateral ventricle anterior horn anterior subependy seen linear enhancement (indicated by the arrow);D:Coronal STIR sequence shows that the left optic nerve is thickened,the signal increased,and optic neuritis changed
图3 22岁女性患者,左眼视力下降1周来诊A:胸段脊髓矢状位T2WI序列扫描可见多发长节段异常高信号影(如箭头所示);B、C:颈段脊髓的T2WI序列矢状位及轴位扫描可见颈髓下段及胸髓上段长节段脊髓炎改变,轴位图像显示病变累及中央部大部分区域(如箭头所示)
Figure 3 A 22-year-old female patient with left eye vision decreased for 1 week A:The thoracic spinal sagittal T2WI sequence scan shows multiple long segment abnormal high signal (indicated by the arrow);B-C:The sagittal and axial scan images of the T2WI sequence of the cervical spinal cord can be seen in the lower cervical spinal cord and the upper segment of the upper thoracic spinal cord.The axial image shows that the lesion affects most of the central region (indicated by the arrow)
4 参考文献
[1] JARIUS S,WILDEMANN B.Aquaporin-4 Antibodies(NMO-IgC)as a Sero logical Marker of Neuromyelitis Optica:A Critical Review of the Literature[J].Brain Pathol,2013,23(6):661-683.
[2] KISTER I,HOWARD J,PERUMAL J,et al.Brain MRI in a series of AQP4-IgG seropositive patients[J].Mult Scler,2010,16:S7-S39.
[3] WINGERCHUK D M,BANWEH B,BENNETT J L,et al.International consensus diagnostic criteria for neuromyelitis option spectrum disorders[J].Neurology,2015,85(2):177-189.
[4] LONGATTI P,PORZIONATO A,BASALDELLA L,et al.The human area postrema:clear-cut silhouette and variations shown in vivo[J].J Neurosurg,2015,122(5):989-995.
[5] NAKAJIMA H,HOSOKAWA T,SUGINO M,et al.Visual field defects of optic neuritis in neuromyelitis optica compared with multiple sclerosis[J].BMC Neurol,2010,10(10):45-51.
[6] JAFIUS S,WILDEMANN B,PAUL F.Neuromyelitis optica:clinical features,immunopathogenesis and treatment[J]Clin Exp Immunol,2014,176(2):149-164.
[7] KUPERSMITH M J,GAL R L,BECK R W,et al.Visual function at baseline and 1 month in acute optic neuritis:predictors of visual outcome[J].Neurology,2007,69(6):508-514.
[8] TUR C,GOODKIN O,ALTMANN D R,et al.Longitudinal evidence for anterograde trans-synaptic degener-ation after optic neuritis[J].Brain,2016,139:816-828.
[9] KIMBROUGH D J,FUJIHARA K,JACOB A,et al.Treatment of neuromyelitis optica:review and recommendations[J].Mult Scler Relat Disord,2012,1:180-187.
[10] KIM S H,HUH S Y,LEE S J,et al.A 5 year follow up of rituximab treatment in patients with neuromyelitis optica spectrum disorder[J].JAMA Neurol,2013,70(9):1 110-1 117.
[11] LEVIN M H,BENNETT J L,VERKMAN A S.Optic neuritis in neuromyelitis optica[J].Prog Retin Eye Res,2013,36(9):159-171.
[12] ASGARI N,LILLEVANG S T,SKEJOE H P,et al. A population-based study of neuromyelitis optica in Caucasians[J].Neurology,2011,76(18):1 589-1 595.
[13] AKAISHIT,NAKASHIMA I,TAKESHITA T,et al.Different etiologies and prognoses of optic neuritis in demyelinating diseases[J].J Neuroimmunol,2016,299:152-157.
[14] BENNETT J L,DE SEZE J,LANA-PEIXOTO M,et al.Neuromyelitis optica and multiple sclerosis:Seeing differences through optical coherence tomography[J].Mult Scler,2015,21:678-688.
[15] TANG W Q,WEI S H.Primary Sjtigren’s syndrome related optic neuritis[J].Int J Ophthalmol,2013,6(6):888-891.
[16] PITTOCK S J,WEINSHENKE B G,LUCCHINETT C F,et al.Neuromyelitis optica brain lesions localized at sites of high aquaporin 4 expreszion[J].Arch Neurol,2006,63:964-968.
[17] CALABRESE M,0H M S,FAVARETTO A,et al.No MRI evidence of cortical lesions in neuromyelitis optica[J].Neurology,2012,79(16):1 671-1 676.
[18] PACHE F,ZIMMERMANN H,FINKE C,et al.Brain parenchymal damage in neuromyelitis optica spectrum disorder-A multimodal MRI study[J].Eur Radiol,2016,26:4 413-4 422.
[19] HUH S Y,MIN J H,KIM W,ET a1.The usefulness of brain MRI at onset in the differentiation of multiple sclerosis and seropositiVe neuromyelitis optica spectrum disorders[J].Mult Scler,2014,20(6):695-704.
[20] KIM H J,PAUL F,LANA-PEIXOTO M A,et al.MRI characteristics of neuromyelitis optica spectrum disorder:An international update[J].Neurology,2015,84(11):1 165-1 173.
[21] CASSINOTTO C,DERAMOND H,OLINDO S,et al.Mlu of the spinal cord in neuromyelitis optica and rccurrent longitudinal extensive myelitis[J].Neuroradiol,2009,36(4):199-205.
[22] ZALEWSKL N I,MORRIS P P,WEINSHENKER B G,et al.Ring-enhancing spinal cord 1esions in neuromyelitis optica spectrum disorders[J].Neurol Neurosurg Psychiatry,2017,88(3):218-225.
[23] SCHMIDT F,ZIMMERMANN H,MIKOLAJCZAK J,et al.Severe structural and functional visual system damage leads to profound loss of vision-related quality of life in patient with neuromyelitis optica spectrum disorders[J].Mult Scler Relat Disord,2017,11:45-50.
[24] BALK L J,STEENWIJK M D,TEWARIE P,et al.Bidirectional trans-synaptic axonal degeneration in the visual pathway in multiple sclerosis[J].J Neurosurg Psychiatry,2015,86:419-424.
[25] COSTELLO F.Optical coherence tomography in neuro-ophthalmology[J].Neurol Clin,2017,35:153-163.
[26] MAT S,LOLLI F.Neuromyelitis optica:An update[J].J Neurol Sci,2011,303:13-21.
[27] PEKCEVLK Y,MITCHELL C H,MEALY M A,et al.Differentiating neuromyelitis optica frpm other causes of longitudinally extensive transverse myeIitis on spinal magnetic resonance imaging[J].Mult Scler,2016,22(3):302-311.
[28] MEALY M A,WINGERCHUK D M,GREENBERG B M,et al.Epidemiology of neuromyelitis optica in the United States:a muhicenter analysis[J].Arch Neurol,2012,69(9):1 176-1 180.
[29] CARROLL W M,FUJIHARA K.Neuromyelitis optica[J].Curr Treat Options Neurol,2010,12(3):244-255.
[30] KIM W,KIM S H,KIM H J,et al.New insinghts into neuromyelitis optica[J].Clin Neurol,2011,7(3):115-127.
(收稿2018-10-10 修回2018-11-10)
本文责编:夏保军
本文引用信息:杨靖,周军,黄立新.磁共振对视神经脊髓炎谱系疾病的诊断价值研究[J].中国实用神经疾病杂志,2018,21(24):2697-2702.DOI:10.12083/SYSJ.2018.24.563
Reference information:YANG Jing,ZHOU Jun,HUANG Lixin.The value of magnetic resonance imaging in the diagnosis of optic neuromyelitis spectrum disease[J].Chinese Journal of Practical Nervous Diseases,2018,21(24):2697-2702.DOI:10.12083/SYSJ.2018.24.563